PCOS and Depression Guide: Understanding the 2026 Connection
Polycystic Ovary Syndrome (PCOS) touches the lives of millions worldwide, yet its deep connection with depression often remains hidden. Many women experience both conditions, but the link is frequently misunderstood or overlooked.
This guide explores the complex relationship between pcos and depression, offering the latest scientific insights and practical strategies for 2026. By understanding this connection, readers can better recognize symptoms and seek effective, holistic care.
Discover cutting-edge breakthroughs, learn about risk factors, and find actionable steps to improve well-being. Empower yourself to take control of your health and be proactive in addressing both PCOS and mental health challenges.
Understanding PCOS: Beyond Hormones
Polycystic Ovary Syndrome (PCOS) is a multifaceted condition that impacts millions of women across the globe. While most people associate PCOS with hormonal issues, its effects are far-reaching, influencing not only physical health but also emotional well-being. Understanding the complexity of PCOS is essential for recognizing its deep connection to mental health struggles, including pcos and depression.
Understanding PCOS: Beyond Hormones
What is PCOS?
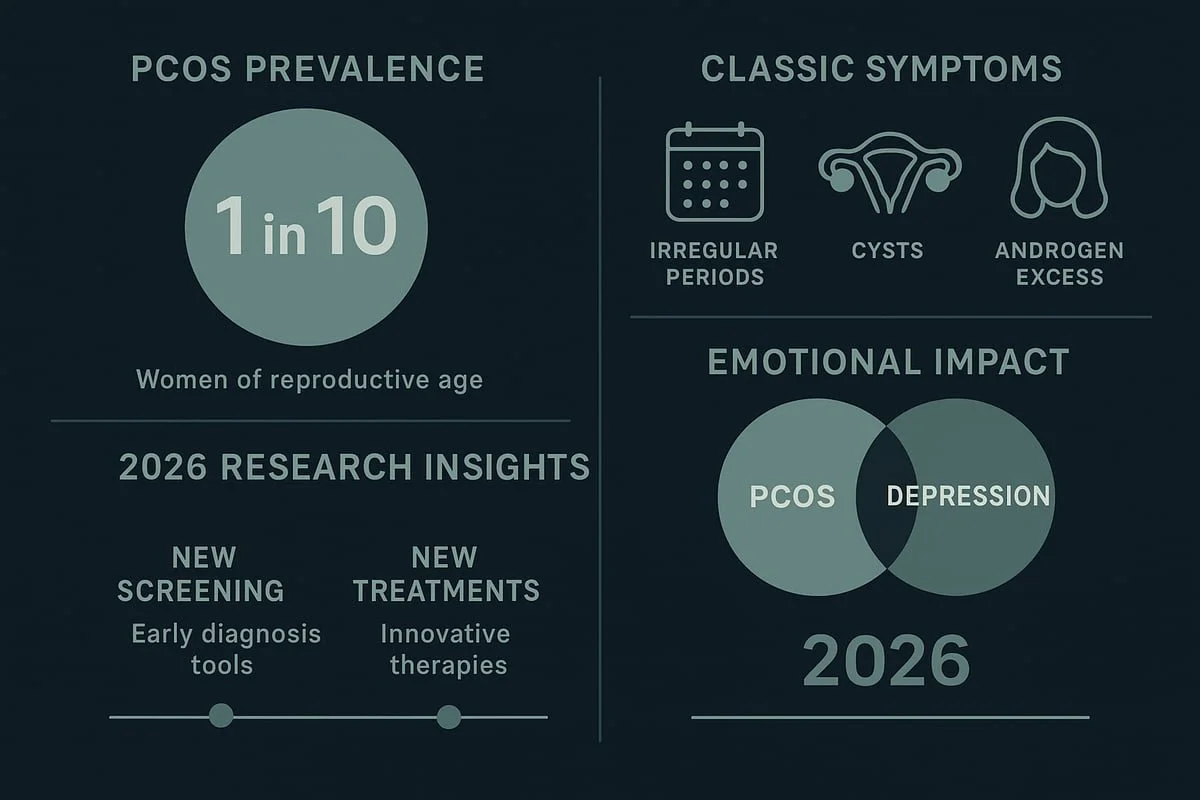
Polycystic Ovary Syndrome, or PCOS, is a common endocrine disorder affecting up to 15 percent of women of reproductive age worldwide. It is characterized by a combination of symptoms, including irregular menstrual cycles, excess androgen production, and the presence of multiple ovarian cysts. Diagnosis is typically based on the Rotterdam criteria, which require at least two out of three hallmark features. PCOS often begins around puberty, though its onset and progression can vary. Common misconceptions suggest PCOS only affects fertility, but its reach extends to metabolic and emotional health, making early recognition vital for preventing complications like pcos and depression. For a comprehensive look at prevalence and mental health impacts, see this systematic review and meta-analysis.
Causes and Risk Factors
The development of PCOS is influenced by a mix of genetic and environmental factors. A family history of PCOS or related metabolic conditions increases risk. Hormonal imbalances, particularly elevated androgens, disrupted insulin signaling, and altered LH/FSH ratios, play a central role. Lifestyle components, including diet, physical inactivity, and chronic stress, also contribute. Obesity and metabolic syndrome are both risk factors and outcomes of PCOS, further complicating the picture. Ethnicity and geography can impact risk levels, with some populations more prone than others. Chronic inflammation and unidentified causes remain under study, revealing why pcos and depression demand ongoing research and tailored prevention strategies.
Physical and Emotional Symptoms
PCOS presents with a broad spectrum of symptoms that can disrupt daily life. Menstrual irregularities and infertility are common physical complaints. Many experience hirsutism, acne, and scalp hair loss due to excess androgens. Weight gain and difficulty losing weight are frequent struggles. Chronic fatigue and sleep disturbances are also prevalent. Equally important are the emotional effects: mood swings, anxiety, irritability, and low self-esteem often accompany physical symptoms. Body image concerns and social challenges can intensify feelings of isolation. These overlapping physical and emotional symptoms highlight why pcos and depression often coexist and why a holistic approach is necessary for care.
PCOS in 2026: New Insights
Recent years have seen significant advances in PCOS research and care. Updated diagnostic tools and biomarkers now allow for earlier, more precise detection. Treatment guidelines are shifting toward patient-centered approaches, recognizing the need to address both physical and mental health. Awareness campaigns and educational initiatives are raising the profile of PCOS globally, while emerging therapies target root causes rather than just symptoms. Mental health is increasingly integrated into PCOS management, reflecting the complex relationship between pcos and depression. Looking ahead, personalized medicine and preventive strategies promise a future where care is tailored to each individual’s unique needs and risk factors.
The Link Between PCOS and Depression
Understanding the connection between pcos and depression is essential for anyone affected by either condition. Research shows that women with PCOS are significantly more likely to experience depression, anxiety, and other mood disorders. Let’s explore the statistics, biological mechanisms, psychosocial factors, and why 2026 is a breakthrough year for awareness and care.
The Link Between PCOS and Depression
Prevalence and Statistics
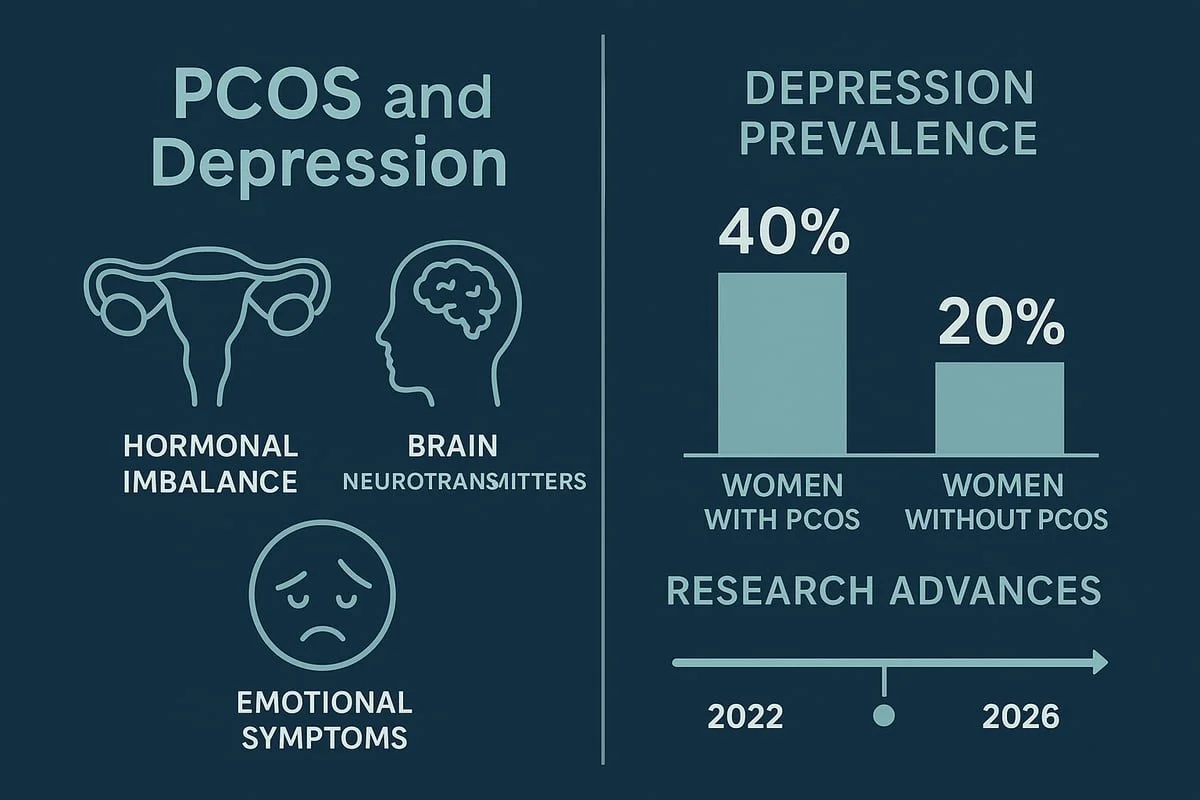
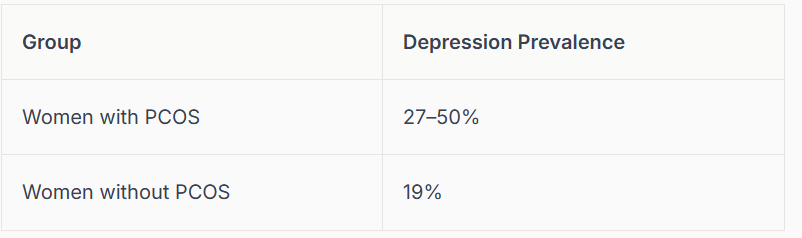
The link between pcos and depression is well documented across global studies. Depression affects between 27% and 50% of women with PCOS, compared to about 19% of women without the condition. Anxiety and mood disorders are also more common, especially among adolescents and young adults.
Here is a quick comparison:
PCOS and Depression Statistics
These numbers highlight a significant mental health gap. Many cases remain undiagnosed due to stigma or lack of screening, increasing the risk of complications. The economic burden is substantial, affecting healthcare systems worldwide. For a deeper dive into these trends, see this PCOS and depression connection resource.
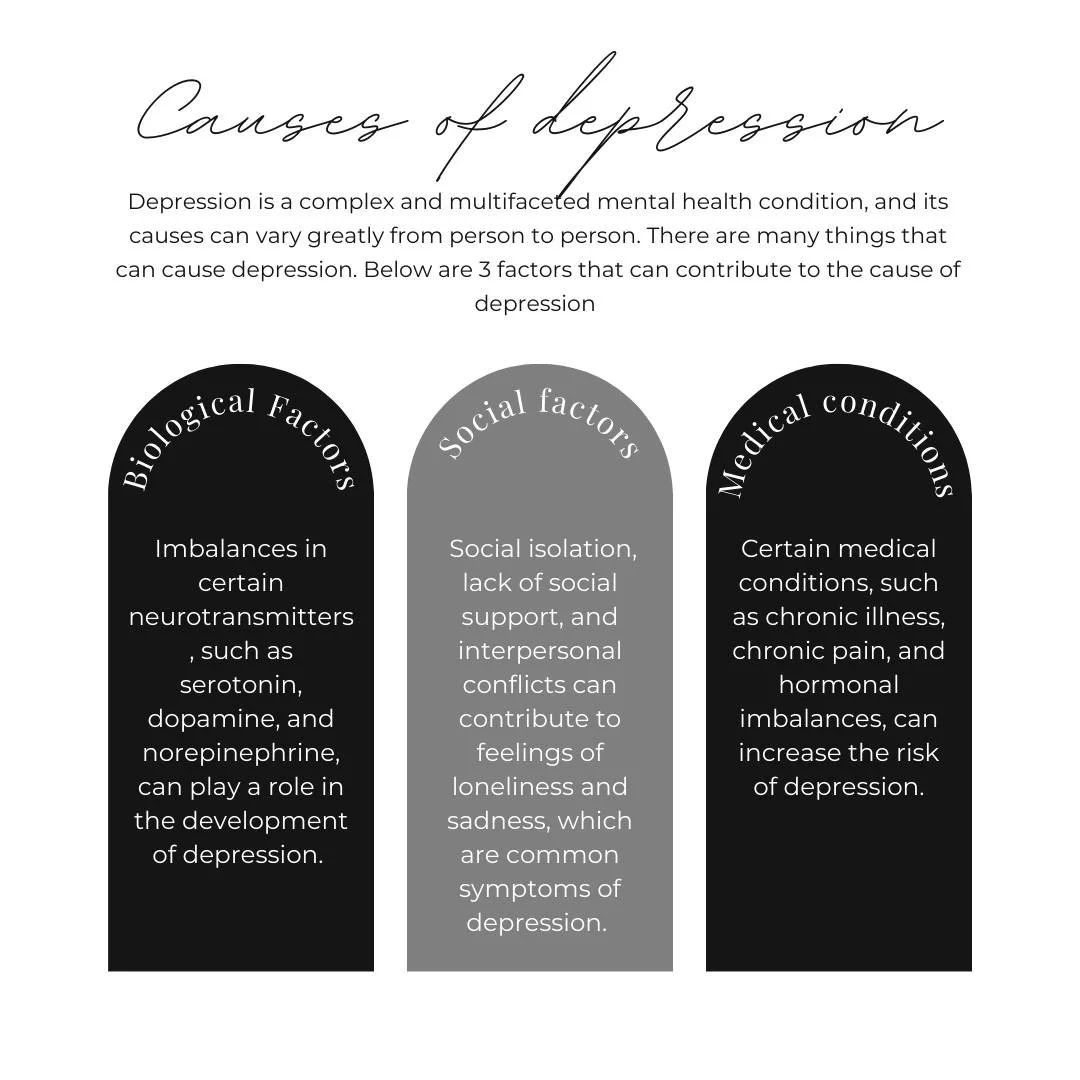
Biological Mechanisms Connecting PCOS and Depression
The relationship between pcos and depression goes beyond surface symptoms. Hormonal imbalances, such as elevated androgens and disrupted estrogen-progesterone cycles, can alter brain chemistry. Insulin resistance, common in PCOS, impacts neurotransmitters like serotonin and dopamine, influencing mood and emotional regulation.
Chronic inflammation and high cortisol levels further disrupt the brain’s stress response. The hypothalamic-pituitary-adrenal (HPA) axis, which controls stress hormones, often becomes dysregulated in PCOS. Recent research also points to the gut-brain axis and the role of the microbiome in mental health for those with pcos and depression.
Sleep disturbances are another factor, as poor sleep affects both hormone balance and mood. This complex interplay makes it clear that treating PCOS requires a holistic approach that addresses both body and mind.
Psychosocial and Lifestyle Factors
Living with pcos and depression involves more than just physical challenges. Many women experience stress from symptoms like hirsutism, acne, and weight gain. These visible changes can lead to social isolation, stigma, and discrimination, further affecting mental health.
Body image dissatisfaction and low self-esteem are common. Relationship difficulties and fertility concerns add to emotional distress. Cultural pressures and limited healthcare access can make it harder to seek support or treatment.
Coping strategies vary. Some women develop adaptive mechanisms, while others struggle with unhealthy behaviors. Addressing these psychosocial factors is crucial for breaking the cycle of pcos and depression and improving overall well-being.
Why 2026 Is a Pivotal Year
The year 2026 marks a turning point in the care of pcos and depression. Increased research funding and new digital mental health tools are making integrated care more accessible. Healthcare systems are adopting models that combine endocrinology and mental health, improving screening and early intervention.
Policy changes are supporting women’s health at a systemic level. Patient advocacy and peer support networks are growing, empowering individuals to share their stories and access resources. As a result, more people are recognizing the signs of pcos and depression earlier and receiving the help they need.
Emerging therapies and personalized medicine are on the horizon, offering hope for better outcomes. In 2026, the focus is on holistic, patient-centered care that addresses both the physical and emotional aspects of PCOS.
Recognizing Symptoms: When PCOS and Depression Coexist
PCOS and depression often occur together, creating a unique set of challenges for those affected. Recognizing when these two conditions coexist is essential for timely intervention and improved quality of life. Understanding the subtle and overt signs can help individuals and healthcare providers take the right steps toward holistic care.
Recognizing Symptoms: When PCOS and Depression Coexist
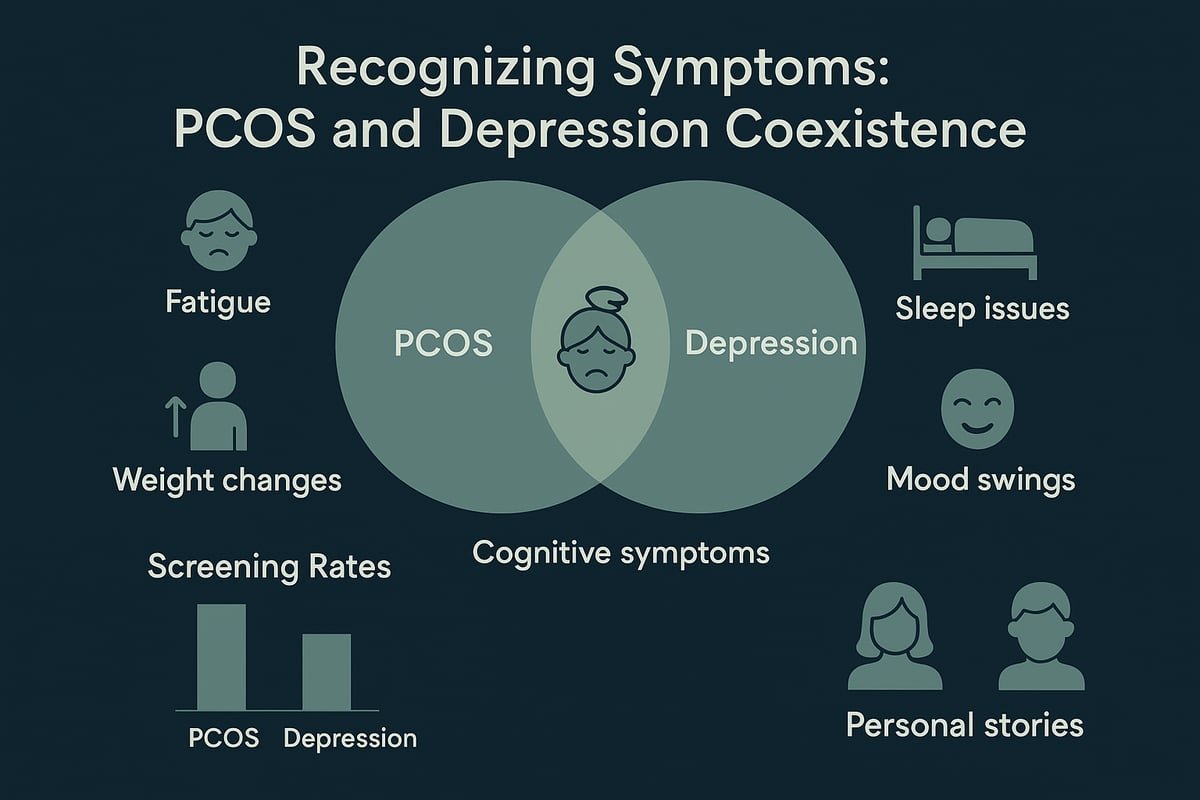
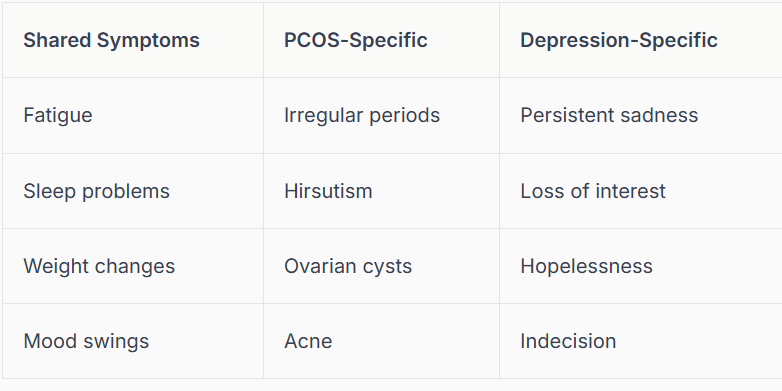
Overlapping and Distinct Symptoms
Many symptoms of PCOS and depression overlap, making it easy to miss the connection. Fatigue, sleep disturbances, and weight changes are common to both, blurring the lines between physical and emotional health. However, some symptoms are distinct.
Physical symptoms linked to PCOS include menstrual irregularities, hirsutism, and acne. Emotional symptoms, such as persistent sadness and hopelessness, are hallmarks of depression. Cognitive issues like difficulty concentrating and indecision may also emerge when pcos and depression are present together.
Tracking symptom patterns helps distinguish between the two. Self-awareness is crucial for recognizing when these conditions coexist and require integrated attention.
Table: Shared vs. Distinct Symptoms
Screening and Diagnosis
Proactive screening is vital when pcos and depression are suspected. Healthcare providers often use tools like PHQ-9 for depression and GAD-7 for anxiety. Gynecologists and primary care teams are increasingly integrating mental health assessments into routine PCOS care.
Screening is especially important for adolescents and young adults, who may face unique mental health challenges. According to a recent meta-analysis, the prevalence of depression and anxiety is significantly higher in young women with PCOS compared to their peers.
Barriers to diagnosis include stigma, lack of awareness, and insufficient mental health resources. Family and partner involvement can support early detection. Telehealth and online screening tools are making it easier to access help and monitor symptoms.
Case Examples and Personal Stories
Personal stories bring the connection between pcos and depression to life. Consider a young woman who struggled with undiagnosed symptoms for years. She faced fatigue, low mood, and social withdrawal, all while managing irregular cycles and acne.
Delayed diagnosis affected her self-esteem and relationships. Once she received integrated care addressing both PCOS and mental health, her quality of life improved. Peer support groups and community forums played a key role in her journey.
These real-life experiences highlight the power of shared narratives. They remind us that open conversations and support networks can empower individuals and reduce isolation.
The Importance of Early Recognition
Early recognition of pcos and depression can make a profound difference. Identifying symptoms before they escalate helps prevent complications like anxiety disorders or disordered eating.
Timely intervention leads to better treatment outcomes and improved adherence to care plans. It also reduces the overall burden on healthcare systems and enhances quality of life for those affected.
Routine mental health screening should be part of every PCOS care plan. Building resilience and coping skills is essential for long-term well-being. Advocacy and education encourage a proactive approach, ensuring more individuals receive the support they need.
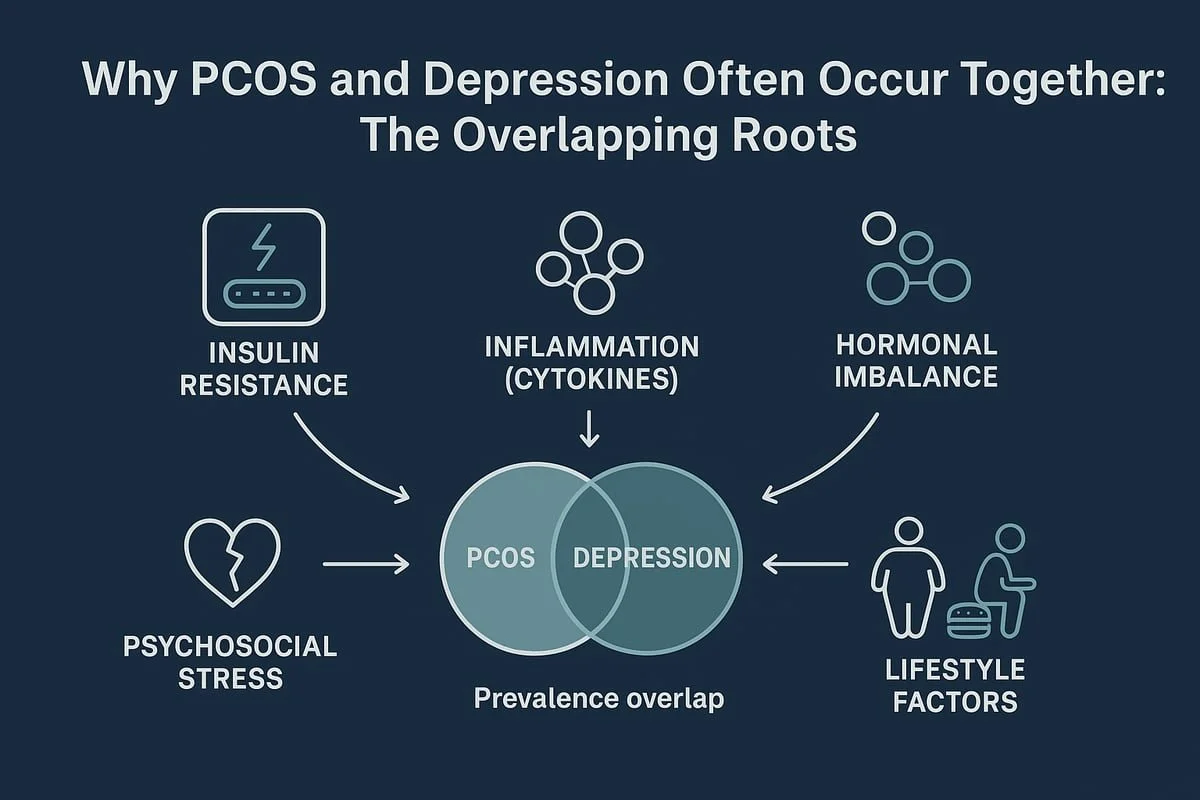
Underlying Causes: Why PCOS and Depression Often Occur Together
Understanding why pcos and depression frequently coexist requires looking beneath the surface. These conditions share overlapping biological, psychological, and lifestyle roots. Each contributes to a cycle that can make symptoms more severe and persistent. Recent research, including a systematic review and meta-analysis, highlights how interconnected reproductive and mental health truly are.
Underlying Causes: Why PCOS and Depression Often Occur Together
Insulin Resistance and Metabolic Dysfunction
Insulin resistance is a core feature in up to 70 percent of women with PCOS. This metabolic disturbance does not just affect blood sugar. It also alters brain chemistry, increasing vulnerability to mood disorders like depression.
Fluctuating glucose levels can trigger fatigue, irritability, and emotional instability. These symptoms overlap with both pcos and depression, creating a feedback loop that is difficult to break. Metabolic syndrome, which often accompanies PCOS, further increases the risk of depressive symptoms.
Early intervention with diet, exercise, and medication improves both metabolic and mental health outcomes. The link between insulin, brain function, and mood remains a key focus of current research.
Chronic Inflammation and Stress Response
Chronic low-grade inflammation is common in PCOS and contributes to the development of depression. Elevated cytokines, the body’s inflammatory messengers, can cross the blood-brain barrier and disrupt neurotransmitter balance.
High cortisol, the primary stress hormone, is frequently seen in both pcos and depression. This creates a cycle where stress and inflammation worsen both conditions over time.
Anti-inflammatory diets, regular physical activity, and stress reduction techniques may help break this pattern. Biomarker testing is emerging as a tool for personalized care, helping to target inflammation’s role in mental health.
Hormonal Imbalances and Neurotransmitters
PCOS is marked by excess androgens, fluctuating estrogen, and imbalanced progesterone. These hormonal changes have a direct impact on neurotransmitters such as serotonin, dopamine, and GABA.
Disruptions in these brain chemicals can lead to mood swings, anxiety, and depressive symptoms. Hormonal therapies are often used to address both physical and emotional symptoms of pcos and depression.
The timing of hormonal changes—such as puberty or postpartum—can be especially challenging. Personalized hormone management is showing promise in stabilizing mood and improving quality of life.
Psychosocial Triggers and Trauma
The visible symptoms of PCOS, like hirsutism and acne, can cause significant emotional distress. Social stigma, shame, and isolation are common, increasing the risk for depression.
A history of trauma or adverse childhood experiences also raises vulnerability to both pcos and depression. Chronic stress and coping fatigue make it harder to manage daily life.
Trauma-informed care and peer support are essential. Community resources can help reduce feelings of isolation and build resilience, making a meaningful difference in mental health outcomes.
Obesity and Lifestyle Factors
Obesity is both a cause and consequence in the pcos and depression relationship. Weight gain is common in PCOS, and facing weight stigma can take a heavy psychological toll.
Physical inactivity, poor nutrition, and sleep disturbances all play a role in worsening symptoms. Addressing these lifestyle factors with exercise, dietary changes, and behavioral therapy can help break the cycle.
Success stories from lifestyle programs show that, with the right support, women can improve both their physical and emotional well-being. Overcoming barriers to healthy living is key for lasting change.
Managing PCOS and Depression: 2026 Strategies for Holistic Care
Navigating pcos and depression in 2026 means embracing a holistic approach. New research and evolving care models empower individuals with actionable strategies for both mind and body. Let’s explore the latest treatments, lifestyle shifts, and support systems designed to address every facet of pcos and depression.
Medical Treatments and Innovations
The landscape for pcos and depression management has rapidly evolved. Standard treatments now integrate endocrinology and psychiatry for optimal outcomes.
Antidepressants, such as SSRIs and SNRIs, are carefully selected for those with pcos and depression, considering hormonal and metabolic factors. Hormonal therapies, including birth control pills and anti-androgens, remain first-line for cycle regulation and androgen excess. Metformin and other insulin-sensitizing agents show dual benefits, supporting both metabolic health and mood stabilization.
Recent clinical trials highlight new medications tailored to individual genetic and metabolic profiles. Providers increasingly use genetic testing to predict drug response and minimize side effects. Collaborative care models mean endocrinologists and mental health professionals work together from diagnosis onward.
The economic impact of untreated pcos and depression is significant, costing billions annually. According to a recent report, the cost of mental health disorders linked to PCOS approached $6 billion in 2021, underscoring the need for integrated medical solutions.
Regular follow-up and symptom monitoring, whether in-person or via telehealth, are now standard. Patients are encouraged to track both physical and emotional symptoms, facilitating timely adjustments to their treatment plans.
Lifestyle Modifications and Self-Care
Lifestyle change is a cornerstone for managing pcos and depression. Nutrition plans focus on anti-inflammatory foods, low-glycemic choices, and the Mediterranean diet, which research shows can stabilize blood sugar and support mood.
Physical activity, including aerobic exercise, resistance training, and mind-body practices like yoga, has proven benefits for metabolic and emotional health. Building a sustainable routine, even with small daily changes, can lead to lasting improvements.
Sleep hygiene is essential. Establishing regular sleep and wake times, limiting screen exposure before bed, and creating a restful environment all support better mood and hormonal balance.
Stress management is equally important. Mindfulness, meditation, and breathing exercises help reduce anxiety and enhance resilience. Digital health tools, such as wellness apps and wearable trackers, allow users to monitor progress and stay motivated.
Many individuals with pcos and depression find success through structured self-care plans. These plans might include meal prepping, joining group exercise classes, or scheduling daily mindfulness breaks. Consistency, not perfection, is key.
Psychological and Emotional Support
Addressing the psychological side of pcos and depression is vital. Cognitive Behavioral Therapy (CBT) remains the most researched and effective approach, focusing on reframing negative thought patterns and building coping skills. Acceptance and Commitment Therapy (ACT) and mindfulness-based therapies are also gaining traction, especially when combined with group support.
Peer networks and group therapy offer validation and shared experience, reducing isolation. Family and partner involvement can enhance recovery, especially when loved ones understand the challenges of pcos and depression.
Body image and self-esteem work are integrated into therapy, helping to combat the emotional toll of physical symptoms. Trauma-informed approaches recognize that many individuals with pcos and depression have histories of adversity. For more on this, see our resource on trauma-aware mental health care, which outlines how personalized support can address deep-rooted stressors.
Teletherapy and online counseling platforms have dramatically increased access, making it easier to find specialized care regardless of location.
Integrative and Complementary Approaches
Many people seek complementary therapies to support conventional treatment for pcos and depression. Acupuncture, herbal medicine, and targeted supplements (such as omega-3s, vitamin D, inositol, and probiotics) have shown promise in symptom relief and overall well-being.
Somatic therapies, including bodywork and breath-based practices, are increasingly used to foster mind-body integration. However, it is crucial to consult qualified practitioners and discuss all supplements or alternative therapies with your healthcare team to avoid interactions.
Combining evidence-based conventional and complementary care delivers the most comprehensive support for pcos and depression. Patient testimonials often highlight improved quality of life when integrative approaches are part of the plan.
Building a Personalized Care Plan
Personalization is the future of pcos and depression care. Collaborative goal setting between the patient and healthcare provider ensures that management strategies fit individual needs, values, and lifestyles.
Tracking symptoms, triggers, and responses to interventions is now easier with digital tools and health apps. These tools support real-time data sharing, enabling quick adjustments to care plans.
Navigating insurance and healthcare systems remains a challenge, but advocacy and education empower individuals to seek integrated, holistic care. Adjusting the plan as life changes ensures ongoing relevance and effectiveness.
Self-advocacy and education are powerful tools. The more you know about pcos and depression, the more confidently you can participate in your care.
Community Resources and Support
Community support is a vital pillar in managing pcos and depression. National organizations, such as PCOS Challenge, offer educational materials, webinars, and advocacy.
Online forums and peer-to-peer platforms provide safe spaces for advice and solidarity. Local support groups can offer in-person connection and shared resources.
Resource directories make it easier to find mental health professionals and PCOS specialists. Community engagement fosters long-term resilience and hope.
When to Seek Professional Help
Recognizing when to seek help is essential for anyone facing pcos and depression. Warning signs include persistent sadness, loss of interest in activities, or thoughts of self-harm.
Finding a qualified provider, such as a gynecologist, endocrinologist, or therapist, is the first step. Prepare for appointments by tracking symptoms and writing down questions.
If care needs are complex, do not hesitate to ask for referrals to multidisciplinary teams. Overcoming stigma and prioritizing mental health can be challenging, but early intervention leads to better outcomes.
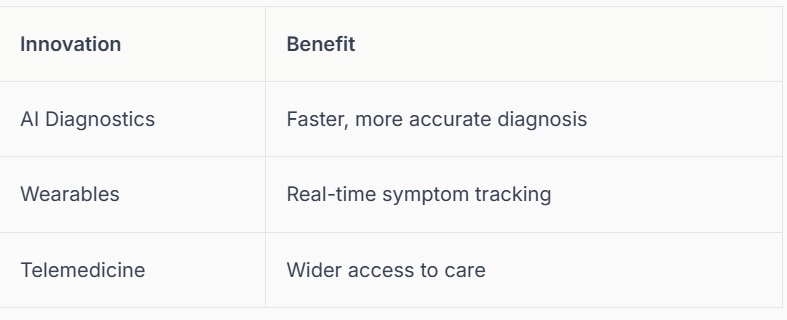
The Future of PCOS and Depression Care: What to Expect by 2026
The future of pcos and depression care is rapidly evolving. By 2026, breakthroughs in technology, policy, and patient advocacy are transforming how women experience diagnosis, management, and support. These changes promise more personalized, integrated, and accessible solutions for those navigating both PCOS and depression.
Advances in Research and Technology
By 2026, research into pcos and depression is driven by AI-powered diagnostics and real-time data sharing. Wearable devices track symptoms such as mood fluctuations and sleep changes, allowing early intervention. Telemedicine expands access to specialists, while genetic and epigenetic discoveries enable tailored treatments. Mental health is now a core feature of women’s health platforms, with patient-led research initiatives shaping priorities. These advances empower women to monitor their health and collaborate with providers more effectively.
Advances in Research and Technology
Researchers continue to explore how technology can improve outcomes for pcos and depression.
Policy, Advocacy, and Awareness
Government and nonprofit organizations are prioritizing pcos and depression in their health agendas. Insurance coverage now often includes mental health services as part of integrated PCOS care. Workplaces and schools are adopting mental health programs, reducing stigma and supporting those affected. Public awareness campaigns, led by patient advocates and influencers, are helping to normalize conversations about PCOS and depression. Community-based research and education initiatives are ensuring that care models reflect real patient needs.
Collaboration among stakeholders is driving more inclusive and equitable care for all.
Personalized and Preventive Approaches
Personalization is reshaping pcos and depression management. Early screening protocols target high-risk adolescents, using predictive analytics to spot symptom flare-ups. Preventive interventions focus on healthy lifestyle habits and family-based programs. Culturally tailored resources recognize the unique needs of diverse populations. Digital coaching and remote monitoring are now standard features, helping individuals stay on track with prevention goals. Success stories from these pilots are inspiring broader adoption.
The future emphasizes prevention, not just treatment, for those with pcos and depression.
Empowerment and Patient-Led Care
Empowerment is central to the 2026 vision for pcos and depression support. Shared decision-making models put patients at the center, with health coaches and navigators guiding their journeys. Self-advocacy training, peer mentorship, and digital storytelling build resilience and community. Patients now have tools to measure outcomes that matter most to them. For those struggling with anxiety or perfectionism, resources such as Perfectionism and anxiety in women provide valuable support.
The rise of patient leadership is shaping a more compassionate and responsive care landscape.
Key Takeaways and Next Steps
The connection between pcos and depression is finally receiving the attention it deserves. Holistic, integrated care models are improving outcomes and quality of life. New tools and resources are available for self-management and support. If you are living with pcos and depression, seek help, share your experiences, and stay informed about the latest advances. Community engagement and advocacy are key to continued progress.
Together, we can build a future where everyone affected by pcos and depression thrives.
Local Support |
PA, NC & SC
Mariah J. Zur | Therapy Intensives in Raleigh, Pittsburgh and across NC, SC, PA
I offer focused therapy intensives for adults who are still functioning but feel worn down by constant pressure, anxiety, or patterns that no longer work. This work is designed for people who want depth, clarity, and relief without labels or long-term weekly therapy. If you’re in North Carolina, South Carolina, or Pennsylvania and curious whether an intensive format could be supportive, you’re welcome to learn more.
Join me on Facebook, Instagram, Pinterest, Google orTikTok for more educational tips, trauma recovery insights, and updates on therapy intensives in Pennsylvania, North Carolina, and South Carolina.
Disclaimer
The content shared here is for educational and informational purposes only. It is not a substitute for psychotherapy, medical care, or individualized mental health treatment. Reading this blog or engaging with my content does not establish a therapeutic relationship.
If you are experiencing significant distress or feel you need personalized support, I encourage you to seek care from a licensed mental health professional in your state. Therapy is deeply personal, and the right support should be tailored to your specific needs, pace, and circumstances.
For adults located in North Carolina, South Carolina, or Pennsylvania who are seeking focused, confidential support, I offer customized therapy intensives designed to address chronic stress, internal pressure, and patterns that no longer work. Information about these services can be found throughout this site.
About the Author
Mariah Zur, LPC is a licensed therapist who works with high-achieving adults navigating chronic stress, internal pressure, and the quiet unraveling that can happen beneath outward success. Her work is especially suited for individuals who are highly functional, deeply self-aware, and exhausted from holding everything together.
Mariah offers therapy intensives for adults seeking focused, contained support without labels, long-term weekly therapy, or unnecessary exposure. Her approach is grounded, relational, and nervous-system informed, helping clients slow the internal spiral, regain a sense of control, and move forward with clarity and steadiness.
She provides intensive therapy services online across North Carolina, South Carolina, and Pennsylvania, with in-person options available in Raleigh, NC.
Credentials
Mariah J. Zur, MS, LPC
Licensed Professional Counselor
Doctoral Student, Counselor Education and Supervision