PCOS Depression Guide: Understanding and Managing in 2026 | NC, SC, PA
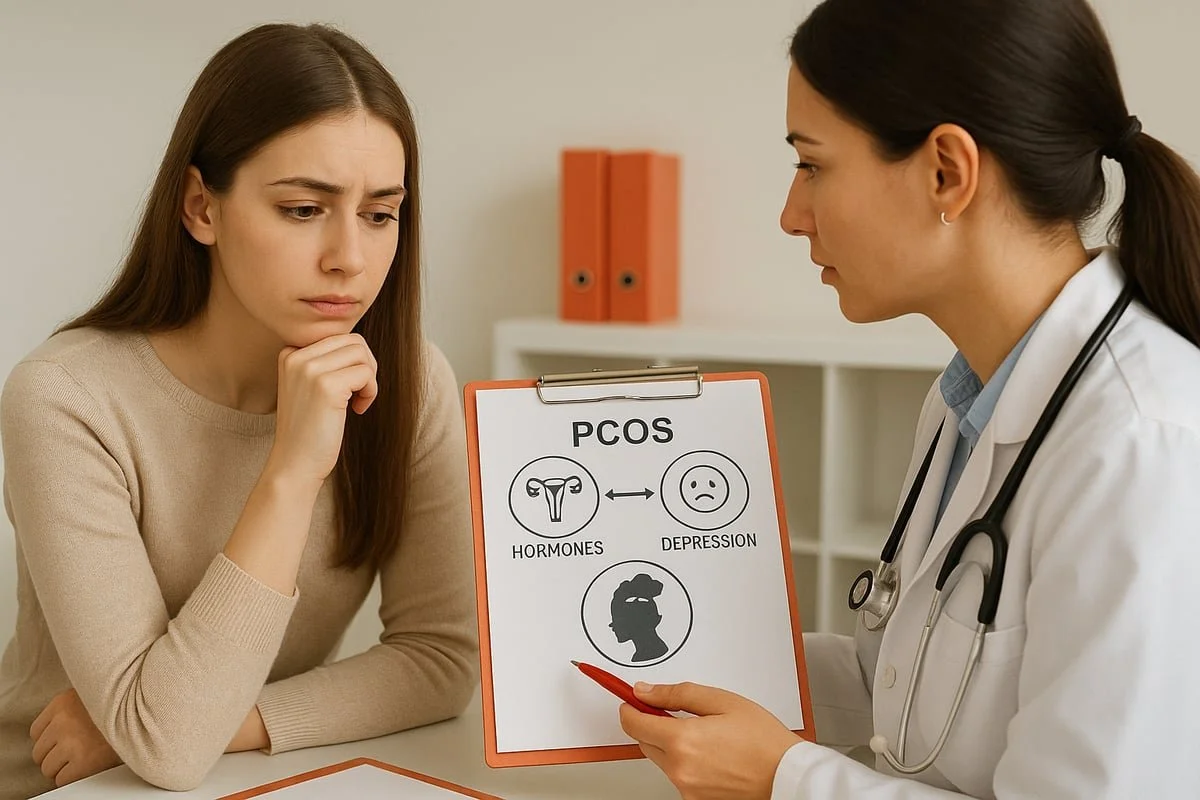
In 2026, the conversation around women's health is changing. More people are recognizing the deep connection between PCOS and depression, yet many still struggle to find effective, compassionate support.
If you or someone you know faces pcos depression, you are not alone. This guide is here to help you understand how these conditions are linked and what you can do about it.
We will break down the latest science, explain why pcos depression is so common, and highlight symptoms and risk factors you should know. You will also find new management strategies and self-care tips backed by experts.
Did you know? PCOS affects millions worldwide, and up to 50% of those diagnosed also experience depression. Want to know why these conditions are so interconnected? Recent research in 2026 is revealing answers that can change your life.
By the end of this guide, you will have the tools and knowledge to manage your symptoms, improve your mental health, and take empowered steps toward a healthier, happier future.
Understanding PCOS and Its Mental Health Impact
Understanding PCOS and It’s Mental Health Impact
Polycystic ovary syndrome (PCOS) is more than a reproductive health issue. For millions worldwide, it shapes both physical and emotional well-being. The close relationship between PCOS and depression is often misunderstood, yet it is a crucial aspect of care in 2026.
What is PCOS?
PCOS is a hormonal disorder affecting women of reproductive age. It is characterized by irregular menstrual cycles, excess androgen levels, and multiple small cysts on the ovaries. About 1 in 10 women globally are diagnosed with PCOS.
The causes of PCOS are complex, involving genetics, insulin resistance, and low-grade inflammation. For example, a young woman might notice severe acne and frequent missed periods, prompting a visit to her doctor. Early recognition of these signs is vital for addressing both the physical and emotional aspects of pcos depression.
Depression in PCOS: The Overlooked Connection
Women with PCOS are significantly more likely to experience depression than those without the condition. Studies show that 27 to 50 percent of women with PCOS report depressive symptoms, compared to 19 percent of women in the general population. For more in-depth data, see this systematic review on depression prevalence in PCOS women.
Depression often goes unrecognized in PCOS, impacting daily functioning and overall quality of life. Imagine a woman with PCOS struggling with persistent sadness and fatigue, unsure if her symptoms are being taken seriously. Recognizing pcos depression early can make a significant difference in long-term outcomes.
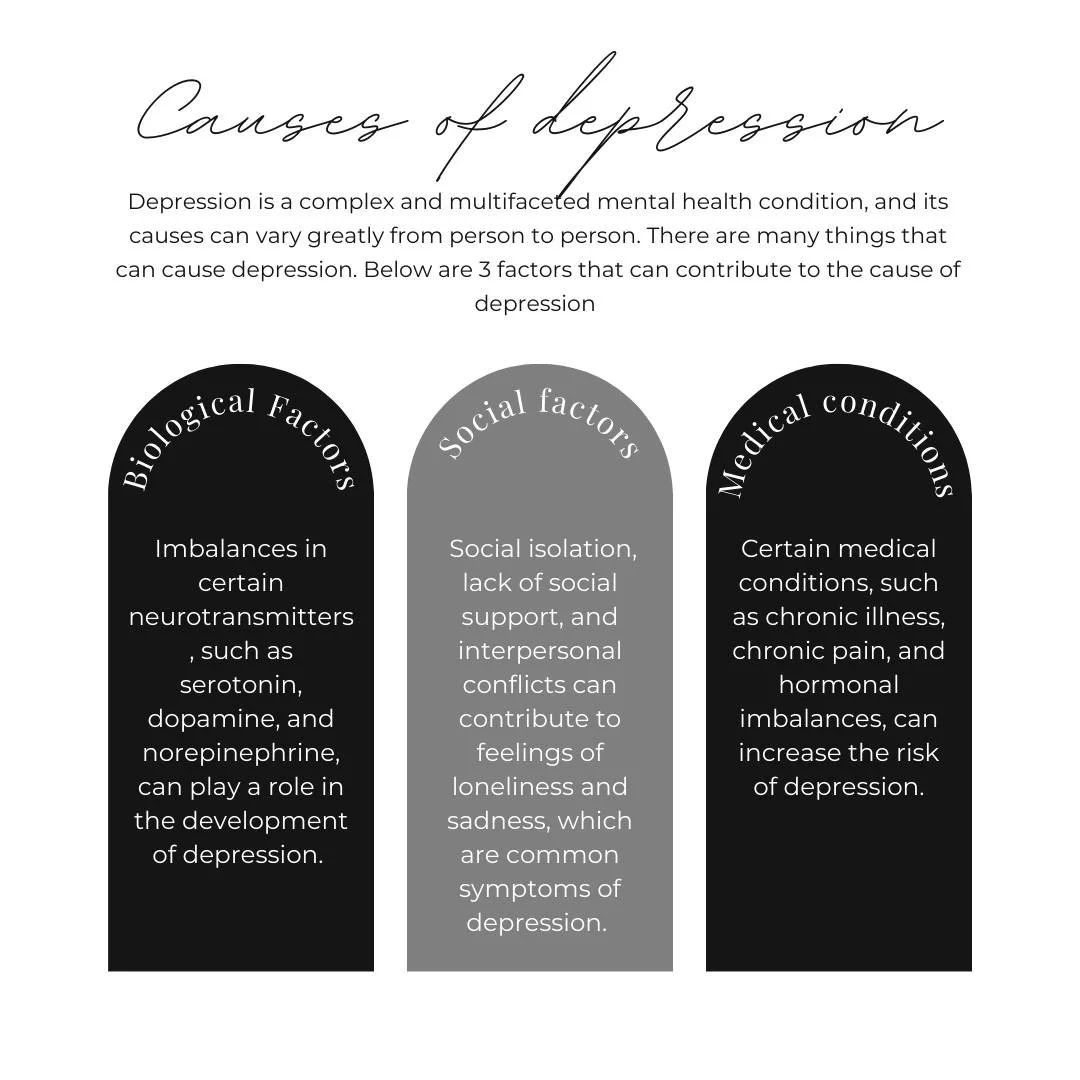
Why PCOS and Depression Often Occur Together
There are several reasons why pcos depression is so common. Biologically, insulin resistance, hormonal imbalances, and chronic inflammation all play a role. On a psychological level, chronic stress, body image concerns, and fears about fertility can deepen emotional distress.
Social factors, including stigma and a lack of support, further complicate the picture. For instance, 70 percent of women with PCOS show insulin resistance, which is linked to mood changes. The stress of managing visible symptoms, like acne or unwanted hair, can lead to both anxiety and depression.
Symptoms of PCOS-Related Depression
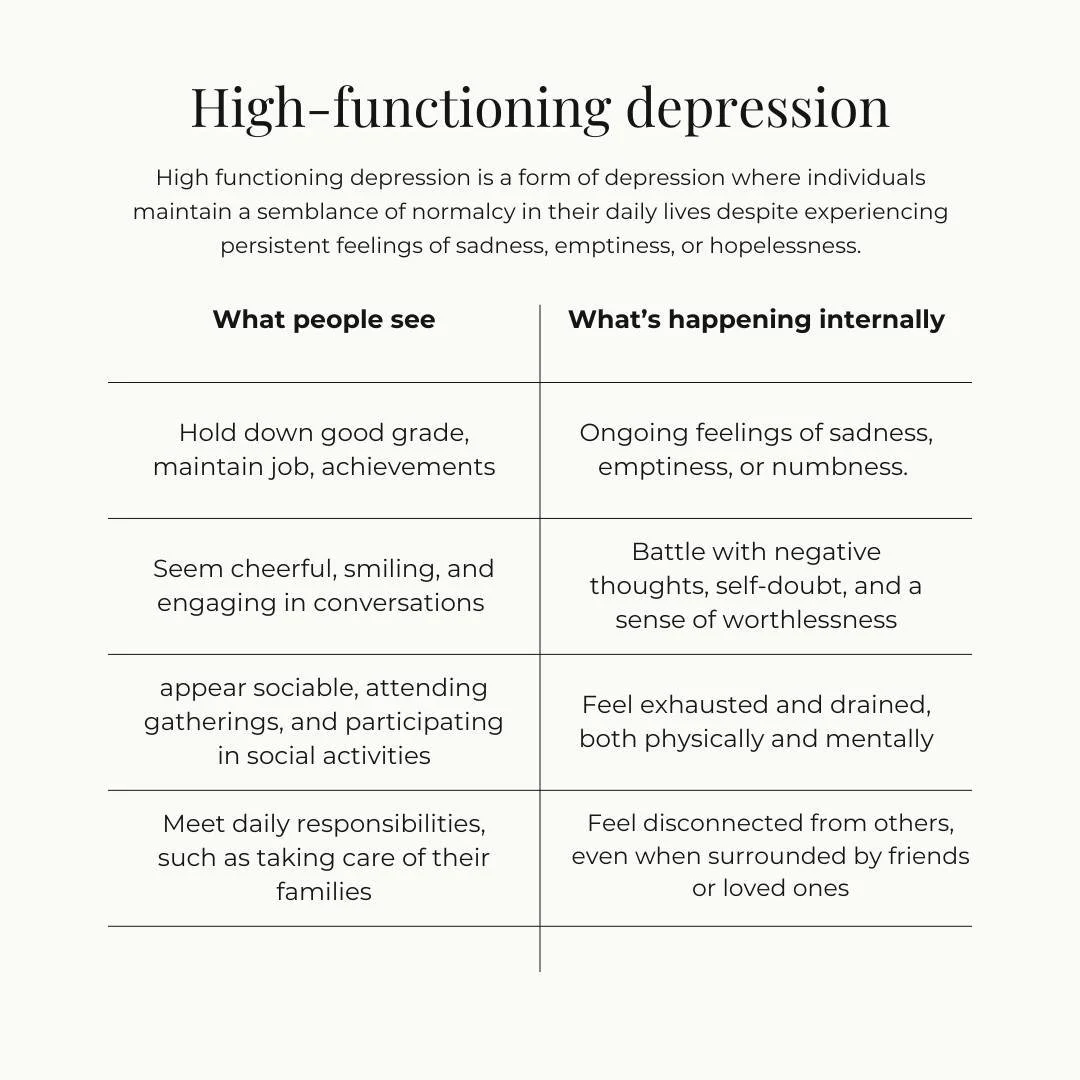
The symptoms of pcos depression can be challenging to distinguish because they overlap with PCOS itself. Emotional signs include persistent sadness, hopelessness, and irritability. Physical symptoms often involve fatigue, sleep problems, and changes in appetite or energy.
Cognitive effects, such as difficulty concentrating or making decisions, are also common. For example, a woman may find it hard to tell if her constant tiredness is due to PCOS or depression. Recognizing these overlapping symptoms is essential for effective treatment and self-care.
Table: Overlapping Symptoms in PCOS and Depression
The Cost of Untreated PCOS Depression
Leaving pcos depression untreated can have serious consequences. It raises the risk of chronic health issues, such as obesity and diabetes. Motivation for self-care and treatment adherence may drop, making physical symptoms worse.
Social withdrawal and strained relationships often follow, especially among younger women. Data shows that rates of anxiety and depression are particularly high in this group. For example, missing work or social events due to mental health challenges can further isolate those with PCOS.
Root Causes: How PCOS Triggers Depression
Root Causes: How PCOS triggers depression
Understanding the root causes behind pcos depression is essential for effective management. Several interconnected biological, psychological, and social factors contribute to this complex relationship. By exploring each layer, we can better grasp why these conditions so often overlap and how targeted strategies can help.
Hormonal and Biological Factors
Hormonal imbalances are a central trigger for pcos depression. Women with PCOS often experience excess androgen levels, which can disrupt mood regulation. High testosterone is linked to increased irritability and emotional instability. Insulin resistance, present in up to 70% of those with PCOS, causes blood sugar swings that can worsen mood and energy levels.
Chronic inflammation is another biological factor. Elevated inflammatory markers and cortisol, the stress hormone, contribute to a prolonged stress response. Research shows women with high androgen levels have a greater risk of developing depressive symptoms. These biological disruptions create a foundation for pcos depression to take hold.
Psychological and Emotional Factors
Living with PCOS can have a profound psychological impact, fueling pcos depression. Body image struggles are common, especially with symptoms like acne, hirsutism, and weight gain. These changes can diminish self-esteem and lead to social withdrawal.
Infertility concerns add another layer of emotional distress. Many women experience anxiety or grief due to uncertainty about their reproductive future. Managing a chronic condition like PCOS is stressful and can feel overwhelming, increasing vulnerability to depression. For example, a patient who battles unwanted hair growth may also struggle with social anxiety, compounding the emotional burden of pcos depression.
Lifestyle and Social Contributors
Lifestyle and social factors play a significant role in pcos depression. Fatigue and low mood may lead to reduced physical activity, creating a cycle that worsens both physical and mental health. Social stigma and misunderstanding from family, peers, or employers can make it difficult to find support.
Barriers to accessing quality care, such as limited mental health services or lack of knowledgeable providers, amplify feelings of isolation. Many women report difficulty connecting with supportive healthcare professionals, which can delay diagnosis and treatment. This lack of support makes managing pcos depression even more challenging.
The Role of Genetics and Family History
Both PCOS and depression often run in families, suggesting a genetic link in pcos depression. Shared risk factors, such as inherited insulin resistance or hormonal imbalances, can make certain individuals more susceptible to both conditions.
Family patterns are frequently observed, with multiple women in the same household experiencing PCOS and mood disorders. If a close relative has a history of depression or PCOS, the risk of developing pcos depression increases. Recognizing these patterns can help with early intervention and support.
Intersection with Other Health Conditions
Comorbid health problems further complicate pcos depression. Obesity is more common in women with PCOS and is independently associated with higher depression rates. Sleep disorders, including insomnia and sleep apnea, are also frequent and can worsen mood and cognitive function.
Other conditions, such as type 2 diabetes and cardiovascular disease, add to the psychological burden. According to a large-scale study linking PCOS to mental health disorders, women with PCOS are significantly more likely to experience depression and anxiety than those without the condition. These overlapping health issues highlight the urgent need for integrated care to address pcos depression effectively.
Diagnosing PCOS-Related Depression in 2026
Diagnosing PCOS-Related Depression 2026
Understanding how to diagnose pcos depression is more critical than ever in 2026. With overlapping symptoms and increased awareness, recognizing the signs early can make a significant difference in outcomes. Let’s break down what to watch for, what the diagnostic process looks like, and how to advocate for your mental health.
Recognizing the Signs: What to Watch For
Spotting pcos depression can be challenging because symptoms often overlap with those of PCOS itself. Fatigue, sleep disturbances, and changes in weight are common in both conditions. However, key red flags include persistent low mood, loss of interest in activities, and social withdrawal.
Healthcare providers use screening tools like PHQ-9 and GAD-7, as well as PCOS-specific checklists, to help identify depression in this population. For example, a patient might report daily sadness and overwhelming fatigue that doesn’t improve with rest.
To help distinguish between burnout and depression, you can read more about the Signs of burnout and depression. Recognizing these nuances is the first step toward effective care.
The Diagnostic Process: What to Expect
Diagnosing pcos depression involves a comprehensive approach. It begins with an initial assessment, where your medical history and current symptoms are discussed. A physical exam will typically follow, focusing on both mental and physical health indicators.
Lab tests, such as hormone panels and blood sugar analysis, help identify underlying PCOS factors that may contribute to mood changes. A mental health evaluation using structured interviews ensures a thorough review of emotional well-being.
Often, effective diagnosis requires collaboration between your gynecologist and a mental health professional. This team approach ensures that both the physical and psychological aspects of pcos depression are addressed together.
Challenges in Diagnosis
There are several challenges when diagnosing pcos depression. One of the most significant is the overlap in symptoms like fatigue, sleep problems, and weight changes. These can easily be mistaken for typical PCOS symptoms, leading to missed diagnoses.
Stigma remains a barrier, as some patients feel hesitant to disclose mental health struggles. Misconceptions may lead to their concerns being dismissed as “just hormonal.” Underdiagnosis is common, especially in busy clinical settings.
A case in point: A woman presenting with mood changes and fatigue may not receive the mental health support she needs if her symptoms are attributed solely to hormonal shifts. Awareness and advocacy are crucial in overcoming these obstacles.
When to Seek Help
Knowing when to seek help for pcos depression is vital. Warning signs include thoughts of self-harm, inability to function in daily life, or experiencing severe distress. Early intervention can prevent symptoms from worsening and improve quality of life.
Open communication with healthcare providers is essential. If you notice persistent sadness, hopelessness, or loss of interest in things you once enjoyed, do not hesitate to reach out. One example is a woman who, after months of worsening symptoms, finally contacts her doctor and begins her journey toward recovery.
Remember, pcos depression is common and treatable. Seeking support is a sign of strength and the first step toward feeling better.
Evidence-Based Strategies for Managing PCOS Depression
Evidence-Based Strategies for Managing PCOS Depression
Effectively managing pcos depression requires a comprehensive, evidence-based approach. New research in 2026 highlights the importance of combining medical, lifestyle, psychological, and holistic strategies. Building a supportive healthcare team can make a profound difference in both symptom management and quality of life.
Medical Treatments: What’s New in 2026
Advances in medical treatments have transformed outcomes for pcos depression. Today, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) remain first-line therapies for depression, but clinicians are now tailoring choices to address PCOS-specific challenges. Hormonal therapies, such as combined oral contraceptives and anti-androgens, help regulate cycles and reduce androgen effects, which may also improve mood. Metformin, long used for insulin resistance, has shown promise in supporting both metabolic and emotional health. Recent studies reveal that integrating hormonal and antidepressant treatments can provide significant relief for those with pcos depression. For example, many women report improved mood and energy when physicians coordinate these therapies.
Lifestyle Modifications for Symptom Relief
Lifestyle changes are a cornerstone in managing pcos depression. Following an anti-inflammatory, low-glycemic diet and maintaining a healthy BMI significantly reduce both physical and emotional symptoms. Regular exercise, such as brisk walking or yoga, improves insulin sensitivity and boosts mood. Prioritizing sleep hygiene is critical, as sleep disturbances are common in PCOS. According to a recent study examining the association between dietary factors, BMI, and depression risk in women with PCOS, dietary improvements can lower depression risk. Many patients find that structured routines, meal planning, and consistent physical activity help stabilize mood and enhance overall well-being with pcos depression.
Psychological and Behavioral Therapies
Therapy is essential in addressing the psychological aspects of pcos depression. Cognitive-behavioral therapy (CBT) is especially effective, focusing on reframing negative thoughts and building coping skills. Acceptance and commitment therapy (ACT) encourages individuals to accept difficult emotions while committing to positive actions. Mindfulness-based interventions, such as meditation and breathing exercises, help reduce stress and improve emotional regulation. These approaches can be tailored to address both the unique challenges of PCOS and the symptoms of depression. For example, engaging in CBT has helped many women manage self-care more consistently and lessen the emotional burden of pcos depression.
Addressing Body Image and Self-Esteem
Body image issues are a significant contributor to pcos depression. Support groups provide a safe space to share experiences and reduce feelings of isolation. Working with a therapist on body image and self-compassion can foster greater self-acceptance. Social media, when used mindfully, connects individuals with positive and empowering communities. Many women have found that participating in PCOS-focused support groups boosts confidence and helps challenge negative self-perceptions. Addressing body image concerns is a vital part of a holistic strategy for managing pcos depression and improving overall quality of life.
Integrative and Holistic Approaches
Integrative therapies are gaining recognition as valuable adjuncts in the management of pcos depression. Supplements such as omega-3 fatty acids, vitamin D, and inositol have shown some promise in supporting mood and hormonal balance, although they should be used under medical supervision. Yoga and meditation help reduce anxiety and promote relaxation, while acupuncture is being studied for its potential benefits in mood regulation and hormonal health. Many patients with pcos depression report that incorporating these holistic strategies alongside conventional care leads to better stress management and improved emotional well-being.
Navigating Healthcare and Building a Support Team
Coordinated care is essential for effective management of pcos depression. A multidisciplinary team—including an endocrinologist, mental health professional, and nutritionist—ensures that all aspects of health are addressed. Advocating for comprehensive treatment plans and regular communication among providers leads to better outcomes. Telehealth options have expanded access to both mental health and PCOS care, making support more accessible than ever. For many, having a dedicated team provides reassurance and continuity, empowering individuals to take control of their pcos depression and work toward lasting recovery.
Self-Care and Coping Strategies for Daily Life
Self-care is a cornerstone in managing pcos depression. Building daily habits that nurture both mind and body can transform how you cope with symptoms and setbacks. By adopting a personalized approach, you can build resilience, protect your mental health, and thrive despite the challenges of pcos depression.
Building Resilience and Emotional Strength
Resilience is not just about bouncing back, but also about growing through challenges. For those living with pcos depression, identifying your unique triggers is crucial. Try keeping a daily journal to track moods and recognize patterns. Creative outlets such as painting or music can provide emotional release and foster positive self-expression.
Incorporate relaxation techniques like deep breathing or progressive muscle relaxation. Many find that somatic practices, such as gentle movement or grounding exercises, can alleviate tension and restore calm. If you are curious about integrating body-based self-care into your routine, explore somatic tools for healing trauma to support emotional resilience.
Practicing self-compassion is vital. Remind yourself that progress takes time, and setbacks are part of the journey. Over time, these steps help build a strong foundation for managing pcos depression.
Managing Relationships and Social Support
Navigating relationships while experiencing pcos depression can be challenging. Communicating your needs clearly with friends and family reduces misunderstandings and fosters empathy. Do not hesitate to express when you need support or space.
Setting healthy boundaries is one of the most powerful self-care tools. Boundaries protect your mental health and prevent emotional exhaustion. For guidance on this topic, read about boundaries to protect mental health and how compassion and boundaries can coexist.
Consider joining a support group, whether locally or online. Sharing experiences with others who understand pcos depression creates a sense of belonging and reduces isolation. Remember, seeking connection is a strength, not a weakness.
Navigating Work, School, and Daily Responsibilities
Coping with pcos depression often means managing fatigue and brain fog during daily tasks. At work or school, do not hesitate to request accommodations like flexible schedules or extra breaks if needed.
Time management strategies can make a big difference. Use planners or digital apps to track assignments and deadlines. Break larger tasks into smaller, manageable steps to avoid overwhelm.
If you find yourself struggling with burnout or exhaustion, prioritize rest and self-care. Recognizing your limits and pacing yourself is essential for long-term success in managing pcos depression. Small adjustments can lead to big improvements in your overall well-being.
Digital Tools and Resources in 2026
Technology can be a valuable ally in your pcos depression self-care plan. Mental health apps now offer mood tracking, guided meditations, and even virtual therapy sessions, all from the privacy of your home. PCOS management platforms allow you to track symptoms and medications, making it easier to spot patterns and share information with your care team.
Online therapy provides greater accessibility and flexibility, especially for those with busy or unpredictable schedules. Many people benefit from using mental health apps to monitor both mood and side effects of treatment.
Embracing digital resources empowers you to take charge of your health. Explore different platforms to find what best fits your needs and lifestyle as you navigate pcos depression.
Preventing Relapse and Maintaining Progress
Sustaining mental health gains with pcos depression requires ongoing attention. Learn to recognize early warning signs, such as changes in mood, sleep, or energy. Regular check-ins with a therapist or support group help maintain accountability and provide encouragement.
Make medical appointments a priority, even when you are feeling well. Consistent symptom monitoring ensures that any setbacks are addressed quickly. Develop a relapse prevention plan, including a list of coping strategies and support contacts.
By staying proactive and connected, you can prevent setbacks and continue building a healthier, more balanced life with pcos depression. Remember, every step forward, no matter how small, is progress.
The Future of PCOS and Depression Care: Trends and Innovations
The landscape of pcos depression care is evolving rapidly as we move into 2026. Emerging research, technology, policy changes, and empowered communities are shaping a future where integrated support is more accessible than ever.
Advances in Research and Treatment
Innovations in treatment are redefining pcos depression management. New medications are being developed to address both hormonal and mood symptoms simultaneously. Researchers are using genetic profiling to create personalized treatment plans tailored to each individual's biology.
Clinical trials are underway to test next-generation antidepressants specifically for women with pcos depression. For example, a 2026 study is investigating a medication that targets both insulin resistance and depressive symptoms, offering hope for more comprehensive care.
New dual-action medications
Genetics-driven therapy plans
Clinical trials for targeted treatments
These advances are expected to improve outcomes and quality of life for those living with pcos depression.
Technology and Telehealth
Technology is transforming how pcos depression is managed and monitored. Telepsychiatry and virtual endocrinology appointments are now widely available, allowing patients to access care from home. Artificial intelligence is used to analyze symptom patterns, predict mood changes, and suggest proactive interventions.
Wearable devices track mood, sleep, and hormonal cycles in real time, giving both patients and providers valuable insights. For instance, a woman with pcos depression can use a wearable to identify mood fluctuations related to her cycle, enabling more precise care.
Virtual appointments for convenience
AI-powered mood prediction
Real-time data from wearables
These technologies are bridging gaps in care and making support more personalized.
Policy and Advocacy
Policy changes are helping to address the economic and social challenges of pcos depression. Increased awareness campaigns and advocacy efforts are leading to more funding for women's mental health research. Insurance coverage is expanding to include integrated pcos depression care, reducing barriers for many people.
Advocacy groups are driving systemic change. New legislation is being introduced to support comprehensive mental health care for people with PCOS. The Mental health costs in PCOS report highlights the urgent need for improved support and funding.
Expanded insurance for integrated care
Funding for research and services
Stronger advocacy and community voice
These developments are paving the way for more equitable and effective pcos depression support.
Empowering Patients: Education and Community
Education and community are central to the future of pcos depression care. Accessible resources help people understand their symptoms, treatment options, and rights. Peer mentoring and patient-led initiatives provide encouragement and practical advice.
Social media is amplifying patient voices and spreading awareness. Viral campaigns challenge stigma and promote self-advocacy, helping people with pcos depression feel seen and supported. Online communities and mentorship programs are fostering resilience and empowerment.
Up-to-date educational platforms
Peer support and mentoring
Social media advocacy and awareness
These efforts ensure that every individual living with pcos depression can find guidance, connection, and hope for the future.
FAQs
PCOS & Depression
1. What is PCOS depression?
PCOS depression refers to depression that occurs alongside polycystic ovary syndrome (PCOS). Hormonal changes, insulin resistance, inflammation, body image struggles, and fertility concerns can all increase the risk of depression in people with PCOS. It’s not “in your head” or a character flaw, it’s a real, treatable mental health concern that deserves care.
2. Why are PCOS and depression so often linked?
PCOS and depression are closely connected because of a mix of biological, psychological, and social factors. Hormonal imbalances, high androgens, and insulin resistance can all affect mood. At the same time, symptoms like weight changes, acne, hair growth, and fertility challenges can impact self-esteem, relationships, and stress levels. Over time, this combo can lead to anxiety, burnout, and depression if it’s not addressed.
3. What are the signs of PCOS-related depression?
Common signs of PCOS-related depression include:
Feeling sad, numb, or hopeless most days
Low energy and extreme fatigue
Sleep changes (sleeping too much or too little)
Brain fog and trouble concentrating
Irritability or feeling “on edge”
Losing interest in things you used to enjoy
Changes in appetite or weight
Feeling like you’re “failing” at managing your health
If you recognize several of these, especially for more than two weeks, it may be depression and not just “PCOS symptoms.”
4. How do I know if it’s burnout or depression from PCOS?
Burnout often shows up as mental exhaustion, cynicism, and feeling drained by responsibilities. Depression tends to run deeper – low mood, hopelessness, loss of interest, and difficulty feeling joy, even during good moments. With PCOS, symptoms overlap, so it’s important to look at how long it’s been happening and how much it’s affecting your daily life. A mental health professional can help you tease apart burnout, anxiety, and depression so you’re not trying to guess alone.
5. Can PCOS depression get better with treatment?
Yes. PCOS depression is highly treatable. Many people feel better with a combination of:
Medical care for PCOS (hormones, insulin resistance, sleep, etc.)
Therapy to address shame, body image, trauma, and chronic stress
Lifestyle changes tailored to energy levels, not perfection
Social support and nervous-system-friendly coping tools
You don’t have to “fix everything” about your body to start feeling better emotionally.
6. What is the best treatment for PCOS depression in 2026?
There isn’t one “best” treatment, but the research points to a combined approach:
Medical care: Hormonal treatment, metformin or other medications for insulin resistance, sleep support, and management of other conditions (like thyroid or blood sugar).
Mental health treatment: Trauma-informed therapy (like IFS, EMDR, CBT, or somatic work) to address shame, perfectionism, anxiety, and old wounds that PCOS can poke at.
Lifestyle and nervous system support: Gentle movement, blood-sugar-friendly nutrition, stress reduction, and nervous-system regulation skills.
Your plan should feel realistic and compassionate, not like another rigid “fix yourself” project.
7. Can therapy really help with PCOS depression if the problem is hormonal?
Yes. Hormones play a huge role, but they don’t tell the whole story. Therapy can help you:
Process the grief, anger, and fear that often come with PCOS
Work through medical trauma, gaslighting, or years of feeling dismissed
Untangle body image, shame, and self-criticism
Build boundaries with work, family, and relationships
Learn regulation tools for anxiety, panic, and overwhelm
It’s not either hormones or mental health—it’s both, together.
8. How is PCOS depression diagnosed?
A provider may:
Review your medical history, PCOS diagnosis, and current symptoms
Use screening tools like the PHQ-9 (for depression) and sometimes GAD-7 (for anxiety)
Ask about sleep, appetite, energy, focus, and mood
Rule out other medical causes (thyroid, vitamin deficiencies, etc.)
For many people, the most accurate diagnosis happens when PCOS care and mental health care talk to each other, not in silos.
9. What can I do at home to help my mood if I have PCOS depression?
Self-help isn’t a replacement for treatment, but it can support your brain and body. A few options:
Eat regular meals to stabilize blood sugar (even simple snacks count)
Move your body gently – walking, stretching, yoga, or dancing in your kitchen
Prioritize sleep routines and wind-down time
Track mood, cycle, and energy to notice patterns instead of blaming yourself
Practice self-compassion: talk to yourself like you’d talk to a close friend with PCOS
If you’ve been white-knuckling it alone, this is your sign you don’t have to anymore.
16. Do you offer online therapy for PCOS depression in PA, NC, and SC?
Yes. I provide virtual trauma therapy and therapy intensives across Pennsylvania, North Carolina, and South Carolina. If you’re dealing with PCOS, depression, burnout, or toxic relationship fallout, we can meet online from your home or office. You can schedule a free consult to see if working together feels like a good fit.
Local Support in PA, NC & SC
If you’re searching for burnout recovery therapy in Philadelphia, a trauma therapist in Pittsburgh, or virtual trauma therapy across North Carolina and South Carolina, you don’t have to keep surviving in exhaustion.
Mariah J. Zur, LPC trauma therapist in Raleigh, Pittsburgh & across PA, NC, SC
I offer personalized trauma therapy intensives designed to help women recover from trauma burnout and toxic relationships—so you can finally feel like yourself again. If rest hasn’t worked, maybe it’s time to try something different. Schedule a consultation today for burnout recovery intensives in PA, NC, or SC.
Join me on Facebook, Instagram, Pinterest, Google orTikTok for more educational tips, trauma recovery insights, and updates on therapy intensives in Pennsylvania, North Carolina, and South Carolina.
Disclaimer
Listen, what you see here on my blog or social media isn’t therapy. It’s here to educate, inspire, and maybe even help you feel a little less alone. But if you’re in it right now and need real support, please reach out to a licensed therapist in your state who can walk alongside you in your healing journey.
Therapy is personal, and you deserve a space that’s all about you. If you’re in Pennsylvania, North Carolina, or South Carolina and looking for a trauma therapist who gets it, I’m currently accepting new clients for customized trauma therapy intensives. Let’s fast-track your healing journey—because you deserve to feel better, sooner.
About the Author
Mariah J. Zur, LPC is a trauma-informed therapist specializing in childhood trauma recovery, narcissistic abuse recovery, burnout, and customized therapy intensives. With over 10 years of experience, Mariah helps women break free from toxic relationship patterns and reclaim their emotional freedom.
She provides virtual trauma therapy intensives across Pennsylvania, North Carolina, and South Carolina, and offers in-person sessions in Pittsburgh, Philadelphia, and Southern Pines, NC. Drawing on evidence-based approaches—including Internal Family Systems (IFS) therapy and somatic strategies—Mariah creates safe, powerful spaces for women ready to do the deep work.
When she’s not in the therapy room, you’ll find her advocating for mental health awareness and supporting women in their personal transformation.
Research Brief Author
Mariah J. Zur, M.S., NCC, LPC, CCTP, PhD in Counselor Education and Supervision Student