Guide to Poverty and Mental Health: Insights for 2026 | NC, SC, PA
In 2026, the invisible connection between poverty and mental health stands out as one of society’s most pressing and misunderstood challenges. Recent statistics show that mental health crises are particularly severe among people experiencing financial hardship.
This guide unpacks how poverty and mental health are deeply intertwined, examines why these issues continue, and shares what can be done to disrupt the cycle. You will explore the complex relationship, see the latest data and trends, and learn about impacts across the lifespan.
Discover actionable insights and strategies, empowering you to advocate for change and find support in the journey ahead.
The Bidirectional Relationship Between Poverty and Mental Health
The Bidirectional Relationship Between Poverty and Mental Health
The connection between poverty and mental health is both profound and complex. This relationship operates in both directions, creating a cycle that can be difficult to break. Understanding how financial hardship and psychological well-being influence each other is critical to addressing both issues effectively.
How Poverty Contributes to Poor Mental Health
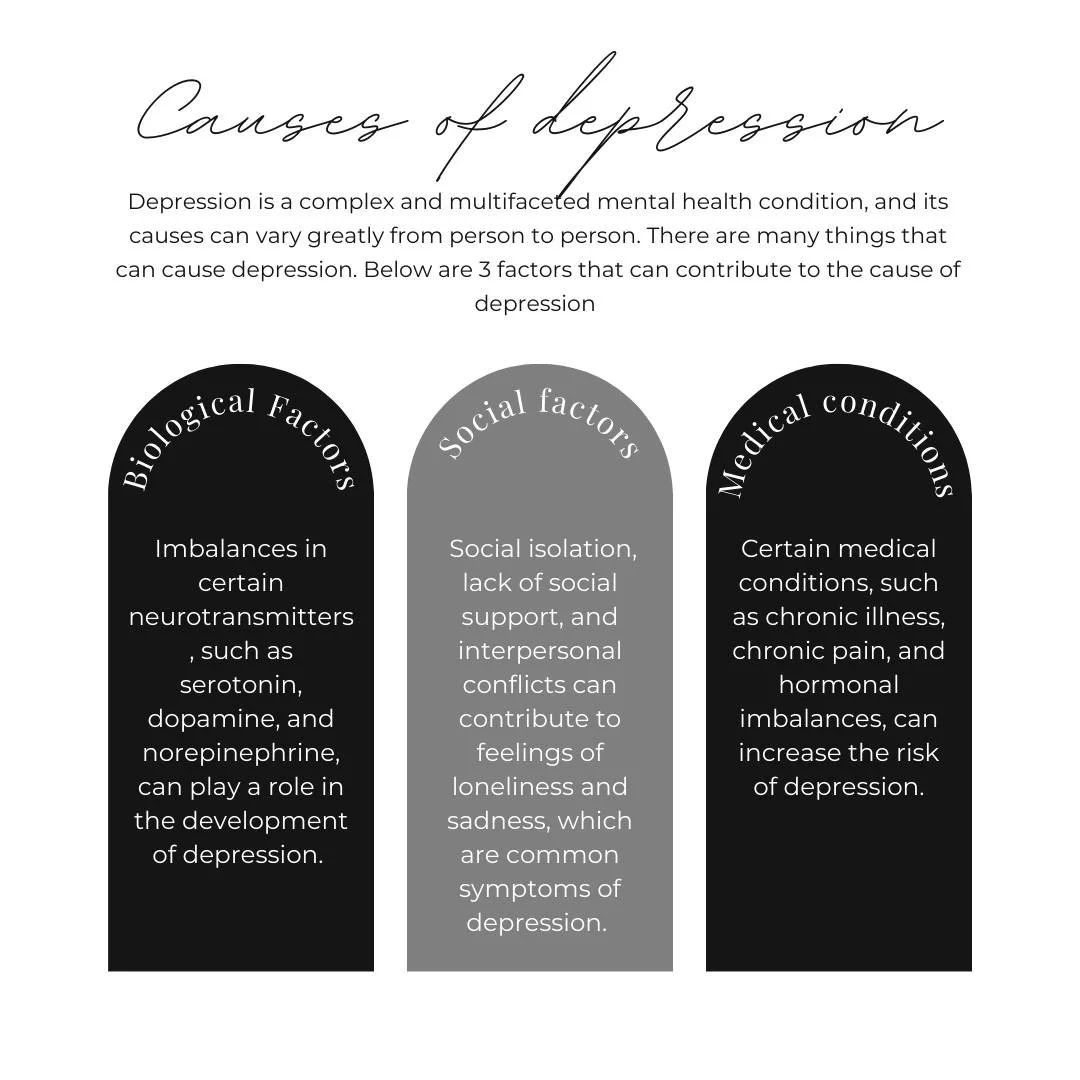
Poverty and mental health are closely intertwined, with chronic financial stress significantly raising the risk of anxiety, depression, and trauma. Individuals living in deprived areas face higher rates of psychiatric disorders. For example, in Scotland’s poorest communities, 23 percent of men and 26 percent of women report mental distress, compared to 12 percent and 16 percent in more affluent regions.
Key factors include:
Social exclusion and lack of opportunity
Unsafe environments and community violence
Poor housing conditions and food insecurity
Children growing up in poverty are especially vulnerable. They experience more abnormal social and emotional difficulties, often linked to adverse childhood experiences. A case in point is Glasgow, where concentrated poverty has led to higher rates of mental health issues among youth. Recent research shows that the timing of exposure to household poverty affects adolescent mental health problems, highlighting the importance of early intervention.
Limited access to healthcare and persistent financial insecurity compound these risks. The effects of poverty and mental health challenges often begin in childhood and continue throughout life.
How Mental Health Problems Can Lead to Poverty
Mental illness can push individuals and families into poverty and mental health struggles can worsen financial situations. When someone experiences a mental health crisis, maintaining consistent employment often becomes difficult, leading to job loss or underemployment.
Additional factors include:
Social withdrawal and weakened support networks
High healthcare costs without adequate insurance
Stigma and discrimination in the workplace
People with serious mental health conditions may face hospitalization or long-term disability, which can further reduce household income. In many urban centers, the cycle of poverty and mental health is evident as those with untreated conditions struggle to access stable housing or education. The impact is not just personal but can lead to generational disadvantages if left unaddressed.
The Vicious Cycle: Complexity and Precarity
The relationship between poverty and mental health is rarely linear. Many individuals move between periods of financial hardship and psychological distress, creating a cycle that is hard to escape.
Consider these compounding challenges:
Precarious employment and unstable housing
Intergenerational transmission of risk
Policy and societal failures that reinforce disadvantage
Data from Scotland reveals that by age seven, nearly 15 percent of children in the most deprived areas have abnormal social or behavioral difficulties, compared to just 3.6 percent in the least deprived. This pattern is not unique to Scotland but is seen internationally, reflecting a global socioeconomic gradient in mental health. Repeated exposure to trauma and cumulative disadvantage make breaking the poverty and mental health cycle especially difficult.
Structural and Environmental Determinants
Beyond individual circumstances, poverty and mental health outcomes are shaped by broader structural and environmental factors. Access to economic, social, and political resources determines whether communities thrive or struggle.
Major determinants include:
Regional disparities, such as Glasgow’s higher mortality rates
Historical factors like deindustrialization and urban policy changes
Area deprivation and the stigma attached to certain neighborhoods
Health behaviors play a role, but they do not explain the root causes. Instead, public policy and social safety nets are critical in influencing both poverty and mental health. Accurate measurement and understanding of deprivation are essential to crafting effective interventions. Recognizing the lived reality behind the statistics is key to developing solutions that work.
Life Course Impacts: Poverty, Adversity, and Mental Health Across the Lifespan
Life Course Impacts: Poverty, Adversity, and Mental Health Across the Lifespan
Poverty and mental health are deeply intertwined throughout every stage of life. The impact of adversity in childhood, transitions in adulthood, cumulative disadvantage in older age, and intersectional risks all shape mental health trajectories. Understanding these life course dynamics is essential to breaking the cycle of disadvantage and building resilient communities.
Childhood and Adolescence
Children growing up in poverty and mental health risk environments face unique challenges from the start. Early exposure to financial insecurity, unstable housing, and limited access to healthcare often leads to developmental delays and emotional difficulties. In Scotland’s most deprived areas, 20% of children are rated as having ‘borderline’ or ‘abnormal’ difficulties by age four.
Adverse childhood experiences such as abuse, neglect, and household dysfunction are far more common in low-income families. For example, 10.8% of children in the lowest-income group report four or more ACEs, compared to just 1% in the highest-income group. These early adversities can have lasting effects, influencing school performance, social relationships, and future prospects.
Longitudinal research, including findings from Glasgow, shows that the impact of how childhood trauma affects adulthood can be profound, making early intervention and family support critical for breaking the poverty and mental health cycle.
Transition to Adulthood and Working Life
The transition from adolescence to adulthood is a critical period for those affected by poverty and mental health challenges. Young people who have experienced hardship often face barriers to higher education and stable employment. Discrimination and stigma in academic and workplace settings can limit opportunities and erode self-confidence.
Premature mortality rates in cities like Glasgow are 30% higher than in comparable UK cities, often linked to substance misuse and deaths of despair. Social isolation and limited support networks further compound these risks.
Mentorship programs, vocational training, and accessible mental health care can help young adults overcome challenges related to poverty and mental health, offering hope for improved outcomes and social mobility.
Older Adults and Cumulative Disadvantage
For many, the effects of poverty and mental health issues accumulate over a lifetime. Older adults with a history of financial hardship are at greater risk for depression, anxiety, and cognitive decline. In Glasgow, men and women in the poorest areas live up to 13.5 and 10.7 years less, respectively, than those in wealthier neighborhoods.
Elderly individuals face compounded challenges, including inadequate housing, limited pensions, and barriers to healthcare. Social isolation is common, often worsened by caregiving responsibilities and family breakdown.
Community support initiatives and age-friendly policies are essential to reduce elder poverty and improve mental health outcomes, helping break the cycle of disadvantage that persists into later life.
Pressure Points and Life Transitions
Critical life events such as homelessness, job loss, bereavement, or family breakdown can trigger or worsen mental health problems, especially for those living in poverty. The cumulative impact of repeated adversity can make recovery more difficult and increase vulnerability to further hardship.
Safety nets, crisis intervention services, and trauma-informed care play a vital role during these transitions. Community and peer support can buffer the effects of adversity, fostering resilience and promoting recovery for individuals experiencing both poverty and mental health stressors.
Intersectionality: Compounded Risks for Marginalized Groups
Individuals with multiple marginalized identities, such as ethnicity, gender, sexuality, and poverty, face compounded risks for poor mental health. Intersectional stigma magnifies barriers to recovery, limiting access to care and support.
Families and communities may experience layered disadvantages, including spatial stigma in deprived urban areas. Research gaps remain in fully understanding these complexities. Advocacy for inclusive, culturally competent services and targeted policy is crucial to address the intersection of poverty and mental health for all.
Stigma, Discrimination, and Social Exclusion
Stigma is an often invisible barrier that reinforces the link between poverty and mental health, shaping how individuals are treated and how they see themselves. Social exclusion, discrimination, and harmful stereotypes can deepen hardship for those already struggling. Understanding how these forces operate is critical to breaking the cycle of disadvantage.
Stigma, Discrimination, and Social Exclusion
The Impact of Stigma on Mental Health and Poverty
Poverty-based stigma is a powerful force that can lead to shame, isolation, and reluctance to seek help. For those facing poverty and mental health challenges, stigma is not just personal, it is structural. It is reinforced by media narratives and public discourse, which can unintentionally create 'spatial' stigma, especially in deprived neighborhoods.
Research shows that experienced poverty stigma is directly linked to poorer mental health, especially among low-income groups. For example, a recent BMC Public Health article on poverty stigma and mental health found a strong association between poverty stigma, food insecurity, and mental health struggles among mothers in disadvantaged communities. People internalize negative stereotypes, leading to lower self-esteem and diminished aspirations.
In cities like Glasgow, stigma contributes to vulnerability, affecting community cohesion and trust. Intersectional stigma, where poverty and mental health overlap with other identities like ethnicity or gender, can magnify these effects. Overcoming this requires understanding that stigma is a fundamental cause of health inequalities, not just an unfortunate byproduct.
Discrimination in Healthcare, Education, and Employment
Discrimination is often experienced in healthcare, education, and the workplace, making it harder for people dealing with poverty and mental health issues to access vital resources. Biases in mental health services can result in misdiagnosis, inadequate treatment, or even denial of care.
In education, students from low-income backgrounds who also struggle with mental health may face lower expectations and reduced access to support. In employment, stigma can mean fewer job offers, limited promotions, and minimal workplace accommodations. Housing and neighborhood resources are also often lower quality for those who are stigmatized.
These barriers create a cycle where poverty and mental health reinforce each other, making recovery and advancement more difficult. Anti-stigma training in public services and clear policy recommendations are essential steps toward equity and inclusion.
Breaking the Cycle: Anti-Stigma Initiatives and Advocacy
Efforts to break the link between poverty and mental health stigma are gaining ground. National and local campaigns, such as Mental Health Awareness Week, are challenging misconceptions and encouraging open conversations. Community-based peer support programs offer safe spaces for sharing experiences and building resilience.
Advocacy organizations play a vital role in policy change, using data-driven approaches to measure and address stigma. Success stories from lived experience demonstrate that targeted interventions can lead to better mental health outcomes. Building alliances across sectors, including education, housing, and healthcare, is crucial for sustainable change.
The voices of those with lived experience are now shaping interventions, ensuring they respond to real needs. As more communities embrace data and evidence, the hope of breaking the cycle of poverty and mental health stigma becomes more tangible.
The Role of Media and Public Perception
Media representation has a powerful influence on how society views poverty and mental health. Negative portrayals can reinforce stereotypes and shape policy in harmful ways. On the other hand, positive storytelling and awareness campaigns can foster empathy and drive social change.
Responsible reporting is essential. Journalists, advocates, and researchers must collaborate to ensure accurate, respectful coverage. Social media platforms, when used thoughtfully, can amplify supportive messages and build networks of solidarity.
Ongoing education for media professionals and the public is needed to challenge misconceptions. Only through sustained effort can we shift perceptions, reduce stigma, and build a more inclusive society.
Systemic Barriers and Policy Challenges
Systemic barriers continue to shape the landscape of poverty and mental health in 2026. Understanding these hurdles is crucial for designing effective solutions that address both root causes and everyday realities.
Systemic Barriers and Policy Challenges
Structural Causes of Inequality
At the heart of poverty and mental health challenges are deep-rooted structural issues. Deindustrialization, austerity policies, and regional economic decline have left lasting impacts on communities.
Access to healthcare, education, and social services remains unequal. Regions like Glasgow experience higher mortality and worse mental health outcomes compared to similar cities, highlighting persistent disparities.
Public policies often fail to address the interconnectedness of poverty and mental health. International comparisons suggest that robust welfare systems and proactive urban policies help reduce these inequalities.
Collaboration between sectors is often lacking, leading to fragmented responses. Addressing root causes, rather than just symptoms, is essential to break the cycle.
Gaps in Mental Health Service Provision
Mental health services remain underfunded and fragmented, especially for those most affected by poverty and mental health issues.
Long wait times, shortages of culturally competent providers, and difficulties in accessing care are common, particularly in deprived or rural areas. People from marginalized backgrounds face additional barriers, such as language and stigma.
Integration between mental health and social care is inconsistent, leaving many without comprehensive support. Workforce shortages and high turnover further strain the system.
According to the WHO report on global mental health conditions, over a billion people worldwide live with mental health conditions, and urgent action is needed to scale up services, especially for disadvantaged populations.
Data, Research, and Measurement Issues
Reliable data is fundamental for addressing poverty and mental health, yet current metrics often fall short.
Underreporting and limited data collection in marginalized groups obscure the true scope of the problem. Few studies capture the intersectional and spatial aspects of stigma that impact both poverty and mental health.
Longitudinal and qualitative research is needed to understand how these challenges evolve over time. Technology and big data offer new opportunities but require careful implementation to avoid reinforcing biases.
Research funding must prioritize community-led and participatory approaches to ensure that lived experiences shape solutions.
Policy Recommendations for 2026 and Beyond
To dismantle systemic barriers, coordinated policy action is essential. Recommendations include:
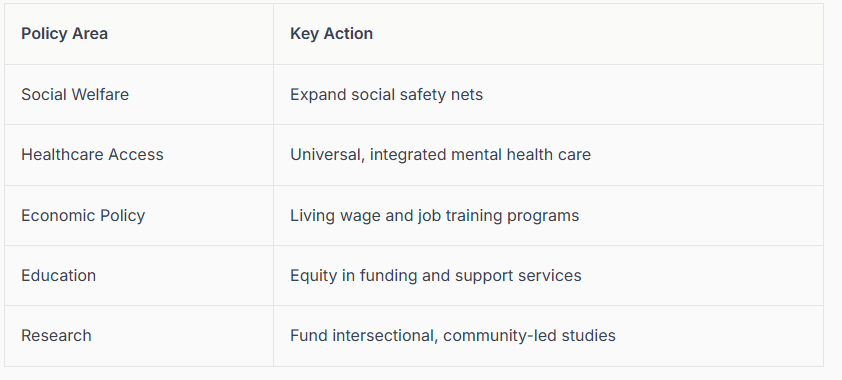
Policy Recommendations Table
Embedding poverty-aware practices into all service commissioning and training is crucial. Advocacy for universal mental health care and stronger collaboration with anti-poverty organizations should remain priorities.
Ongoing monitoring, accountability, and data-driven evaluation will help ensure that progress on poverty and mental health is both measurable and sustainable.
Innovative Strategies for Prevention, Intervention, and Support
Breaking the cycle of poverty and mental health requires bold, evidence-based strategies. In 2026, prevention, intervention, and support must go beyond traditional approaches. By integrating early action, trauma awareness, community engagement, digital access, and policy reform, communities can address the root causes and provide pathways to resilience.
Early Intervention and Family Support
Early intervention is a cornerstone of breaking the link between poverty and mental health. Universal mental health screenings in schools and primary care settings can identify issues before they escalate. Targeted family support, especially in deprived areas, addresses the compounding stressors that contribute to poor outcomes.
Parenting programs and trauma-informed early childhood education foster resilience in children facing adversity. Community-based prevention initiatives, such as home visiting and family resource centers, create safe spaces for families to access support.
Evidence consistently shows that early intervention reduces the risk of adult mental illness. For a deeper dive on interrupting cycles of trauma and disadvantage, see Breaking Generational Trauma Patterns. Integrating social services with mental health care ensures families receive holistic support.
Trauma-Informed and Culturally Competent Care
Adopting trauma-informed practices is essential for effective poverty and mental health interventions. Providers trained to recognize complex trauma can tailor care to each individual's history and needs. This approach is particularly vital in communities with high rates of adverse childhood experiences.
Culturally competent care ensures that interventions respect and reflect the diverse backgrounds of those affected by poverty and mental health issues. Peer support models, where individuals with lived experience guide others, build trust and engagement.
Urban clinics that implement trauma-informed methods often report improved outcomes, reduced stigma, and better access for marginalized groups. Ongoing evaluation and adaptation of care models help address evolving needs and barriers.
Community Development and Social Movement Building
Empowering communities is key to transforming poverty and mental health outcomes. Grassroots initiatives, such as food banks, housing cooperatives, and mental health collectives, directly address social determinants of health.
Building social capital within neighborhoods increases resilience and fosters a sense of belonging. Partnerships between public health agencies, schools, and local organizations amplify impact and sustainability.
In Glasgow, for example, community-led mental health programs have demonstrated success in reducing isolation and improving well-being. Advocacy for policy change and mobilization of local resources are vital for long-term progress.
Digital and Peer Support Innovations
Digital technology is reshaping access to poverty and mental health support. Telehealth platforms and online peer support groups make care more accessible, especially in rural or underserved areas.
Peer-led crisis intervention services provide immediate, relatable assistance. Data shows that digital channels often reduce stigma and increase engagement, complementing traditional services.
To ensure equity, strategies must address the digital divide and protect privacy. Integrating digital innovations with face-to-face care offers a holistic approach to support, meeting people where they are.
Prevention Through Policy and Economic Empowerment
Policy and economic reforms are powerful tools for addressing poverty and mental health. Living wage policies, income supports, and affordable housing initiatives act as preventative measures, reducing psychological distress at the population level.
Universal healthcare access, educational equity, and job training programs create upward mobility and stability. Anti-discrimination laws help break down barriers for those facing stigma and marginalization.
Evidence from the NBER study on poverty and health underscores the impact of economic interventions on mental health outcomes. Collaboration with employers and community stakeholders ensures that policies translate into real-world improvements.
Building a Roadmap for Change: Insights for 2026
A future where poverty and mental health do not reinforce each other is possible, but it requires coordinated action at every level. By understanding the complexity of these issues, we can chart a course toward meaningful change. Building this roadmap means learning from what works, empowering people, and embracing innovation.
The Importance of Multi-Level Solutions
Tackling poverty and mental health demands a multi-level approach. No single intervention can address such deeply intertwined issues. Integrated strategies that link individual support, community action, and policy reform are essential.
For example, combining early intervention programs with community-led projects and responsive policies amplifies impact. Recent public health emergencies have shown the value of rapid, cross-sector collaboration. Leaders who prioritize data, evaluation, and continuous improvement can set achievable goals and measure progress.
Consider how Somatic Tools for Generational Trauma are informing interventions that break cycles of adversity. These models show how addressing trauma at multiple levels leads to better outcomes for those impacted by poverty and mental health challenges.
Empowering Individuals and Families
Empowerment is vital in the roadmap for addressing poverty and mental health. Individuals and families need access to accurate information, practical tools, and supportive networks.
Key resources include:
Mental health helplines and peer mentorship
Financial counseling and legal aid
Family resilience and self-advocacy workshops
Stories of recovery highlight the power of community and lived experience. Accessible services and peer support can help people navigate challenges and reduce stigma. For those experiencing chronic stress, Burnout Recovery After Trauma offers guidance on rebuilding well-being and finding sustainable support.
The Role of Advocacy, Research, and Lived Experience
Advocacy and research are pillars of progress. Policy and program design must center the voices of those with lived experience of poverty and mental health struggles. Advocacy organizations play a crucial role in closing knowledge gaps and pushing for systemic reform.
Participatory research, where communities drive the questions and solutions, leads to more relevant and sustainable outcomes. Data-driven storytelling and coalition-building are vital tools for keeping the issue in the public eye and holding institutions accountable.
Supporting training and capacity-building for advocates ensures that the movement for change remains strong and adaptive. Ongoing evaluation and transparent reporting help maintain momentum and credibility.
Looking Ahead: Trends and Opportunities for 2026
Looking forward, momentum is building for systemic transformation in poverty and mental health. Advancements in technology are improving access to care, while global research is deepening our understanding of intersectionality and trauma.
International collaboration is fostering new solutions. Shifts in economic and social policy are opening doors for prevention and empowerment. Communities are increasingly recognized as key partners in designing and delivering support.
By focusing on evidence-based approaches, embracing innovation, and prioritizing hope, we can create a future where poverty and mental health no longer reinforce each other. The roadmap requires persistence, adaptability, and a shared commitment to progress.
Poverty and Mental Health FAQ
1. What is the relationship between poverty and mental health?
Poverty and mental health have a bidirectional relationship: living in poverty increases the risk of anxiety, depression, trauma, and substance use, while untreated mental health problems can make it harder to work, study, or keep stable housing. Over time, this creates a cycle where financial stress and psychological distress feed each other.
2. How does poverty cause mental health problems?
Poverty contributes to poor mental health through:
chronic financial stress and uncertainty
unsafe housing, neighborhood violence, or instability
food insecurity and lack of basic resources
limited access to quality healthcare and mental health services
Children and adults in low-income communities are more likely to experience adverse childhood experiences (ACEs), chronic stress, and trauma, all of which increase risk for depression, anxiety, and PTSD across the lifespan.
3. Can mental health problems lead to poverty?
Yes. Mental health challenges can:
make it hard to maintain steady employment or schooling
lead to job loss, underemployment, or disability
increase healthcare costs and debt
strain relationships and support systems
When symptoms go untreated, people are more vulnerable to housing instability, financial hardship, and long-term economic disadvantage.
4. Why is poverty and mental health called a “vicious cycle”?
It’s called a vicious cycle because:
Poverty increases mental health risk (through stress, trauma, and deprivation).
Mental health symptoms make it harder to escape poverty (through lost income, low energy, and stigma).
Structural factors, like underfunded services, discriminatory policies, and regional inequality, keep that loop going.
Without early intervention, trauma-informed care, and policy change, the cycle tends to repeat across generations.
5. What can I do if I’m dealing with both financial stress and mental health symptoms?
If you’re juggling money stress and mental health symptoms, you’re not “failing”—you’re living in conditions that overload nervous systems. Helpful steps can include:
reaching out for low-cost or sliding scale counseling
using community resources (food banks, legal aid, housing support, crisis lines)
practicing nervous-system regulation tools to manage overwhelm
connecting with peer support or advocacy groups that understand poverty and mental health
You deserve care that honors both your emotional reality and your material reality, not one or the other.
Local Support in PA, NC & SC
If you’re searching for burnout recovery therapy in Philadelphia, a trauma therapist in Pittsburgh, or virtual trauma therapy across North Carolina and South Carolina, you don’t have to keep surviving in exhaustion.
Trauma therapist in Raleigh, Pittsburgh and across NC, SC, PA.
I offer personalized trauma therapy intensives designed to help women recover from trauma burnout and toxic relationships—so you can finally feel like yourself again. If rest hasn’t worked, maybe it’s time to try something different. Schedule a consultation today for burnout recovery intensives in PA, NC, or SC.
Join me on Facebook, Instagram, Pinterest, Google orTikTok for more educational tips, trauma recovery insights, and updates on therapy intensives in Pennsylvania, North Carolina, and South Carolina.
Disclaimer
Listen, what you see here on my blog or social media isn’t therapy. It’s here to educate, inspire, and maybe even help you feel a little less alone. But if you’re in it right now and need real support, please reach out to a licensed therapist in your state who can walk alongside you in your healing journey.
Therapy is personal, and you deserve a space that’s all about you. If you’re in Pennsylvania, North Carolina, or South Carolina and looking for a trauma therapist who gets it, I’m currently accepting new clients for customized trauma therapy intensives. Let’s fast-track your healing journey—because you deserve to feel better, sooner.
About the Author
Mariah J. Zur, LPC is a trauma-informed therapist specializing in childhood trauma recovery, narcissistic abuse recovery, burnout, and customized therapy intensives. With over 10 years of experience, Mariah helps women break free from toxic relationship patterns and reclaim their emotional freedom.
She provides virtual trauma therapy intensives across Pennsylvania, North Carolina, and South Carolina, and offers in-person sessions in Pittsburgh, Philadelphia, and Southern Pines, NC. Drawing on evidence-based approaches—including Internal Family Systems (IFS) therapy and somatic strategies—Mariah creates safe, powerful spaces for women ready to do the deep work.
When she’s not in the therapy room, you’ll find her advocating for mental health awareness and supporting women in their personal transformation.
Research Brief Author
Mariah J. Zur, M.S., NCC, LPC, CCTP, PhD in Counselor Education and Supervision Student