Bipolar Schizophrenia Versus: Key Differences in 2026
Are bipolar disorder and schizophrenia truly so different, or are they still being confused in 2026’s fast-evolving mental health landscape? The question of bipolar schizophrenia distinctions remains a critical concern for patients, families, and clinicians alike. This article explores the latest understanding, breaking down their symptoms, causes, diagnostic challenges, treatments, and the unique lived experiences of those affected.
Confusion and stigma persist, often leading to myths and misdiagnoses. By clarifying the key differences, we aim to empower you with accurate information. Learn and share these facts to foster greater awareness, support, and improved outcomes for everyone touched by these conditions.
Understanding Bipolar Disorder in 2026
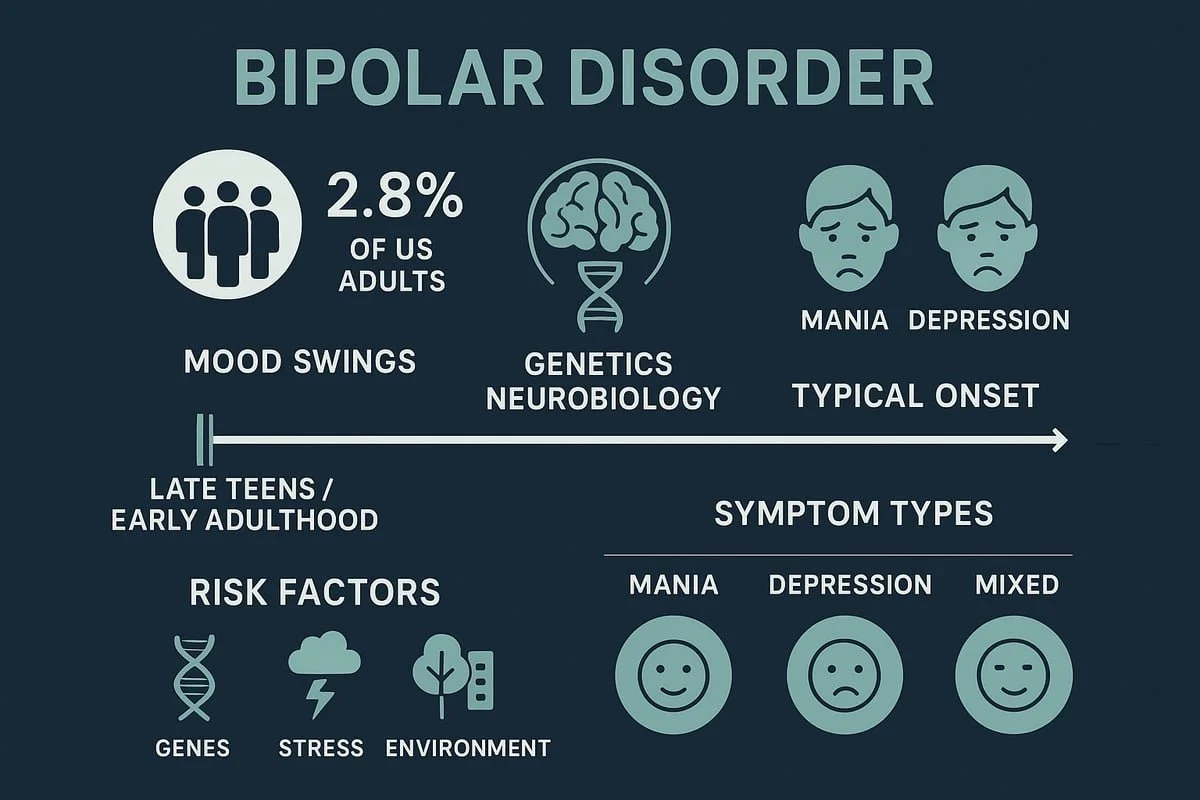
Bipolar disorder stands out as one of the most widely discussed mood disorders today, especially in conversations comparing bipolar schizophrenia. The condition is defined by dramatic shifts in mood, energy, and activity levels that can disrupt daily life. Recent studies estimate that about 2.8% of adults in the United States are affected each year (CDC, 2025).
Daily functioning, relationships, and work can be deeply impacted by bipolar disorder. Advances in brain imaging and genetics have expanded our understanding, highlighting differences between bipolar schizophrenia and other diagnoses. For example, a high-achieving professional may swing from periods of intense productivity and little need for sleep to weeks of severe, immobilizing depression.
Understanding Bipolar Disorder in 2026
Defining Bipolar Disorder
Bipolar disorder is a chronic, recurring mental health condition marked by episodes of mania or hypomania and depression. Unlike bipolar schizophrenia, which is often confused due to overlapping symptoms, bipolar disorder centers on mood instability. The disorder affects nearly 2.8% of U.S. adults each year, with many facing challenges in relationships, work, and daily routines.
Recent research has shed light on the neurobiological underpinnings, revealing changes in brain structure and function. Genetics also play a key role, as do environmental stressors. For instance, a person may experience weeks of boundless energy and creativity, followed by a period of deep sadness and withdrawal.
Types and Symptoms of Bipolar Disorder
There are several forms of bipolar disorder, each with unique patterns. Bipolar I involves at least one manic episode, often paired with depressive episodes. Bipolar II requires at least one hypomanic episode and one major depressive episode. Cyclothymic disorder describes chronic, fluctuating mood disturbances that never meet full criteria for mania or depression.
Symptoms include:
Mania: Euphoria, impulsivity, racing thoughts, decreased need for sleep
Depression: Hopelessness, fatigue, difficulty concentrating, suicidal thoughts
Mixed features: Agitation and despair at the same time
Up to 60% of people with bipolar disorder may experience psychotic symptoms during severe episodes, which can blur the lines between bipolar schizophrenia. In 2024, the FDA approved Fanapt for manic and mixed episodes in Bipolar I, reflecting ongoing advances in treatment (FDA approves Fanapt for bipolar disorder).
Causes and Risk Factors
Research into bipolar schizophrenia highlights the complex interplay of genetics, neurobiology, and environment in bipolar disorder. Having a first-degree relative with the condition raises one’s risk by 10-25%. Neurotransmitter imbalances, particularly involving dopamine and serotonin, have been implicated.
Environmental triggers also matter. Traumatic experiences, major life transitions, and substance use can all contribute. The stress-diathesis model explains how inherited vulnerability interacts with stressors to trigger episodes. New findings point to inflammation and the gut-brain axis as emerging areas of interest.
Course, Prognosis, and Complications
Bipolar disorder typically begins in the late teens or early adulthood, a period also critical for differentiating from bipolar schizophrenia. The course is often episodic, with periods of wellness between episodes, but it can become progressive without treatment.
Complications are common:
Substance abuse affects up to 50% of individuals.
Suicide risk is significant, with 15-20% attempting at some point.
Delays in diagnosis often worsen outcomes.
Long-term prospects are brighter with early intervention and consistent treatment. For many, recognizing the early signs and seeking help is the key to managing bipolar disorder and avoiding the pitfalls that can lead to confusion with bipolar schizophrenia.
Understanding Schizophrenia in 2026
Schizophrenia is one of the most challenging mental health conditions to understand and treat. In 2026, new research and technology are reshaping how clinicians distinguish schizophrenia from other disorders like bipolar schizophrenia. Let’s explore the latest insights into its definition, symptoms, causes, and outcomes.
Understanding Schizophrenia in 2026
Defining Schizophrenia
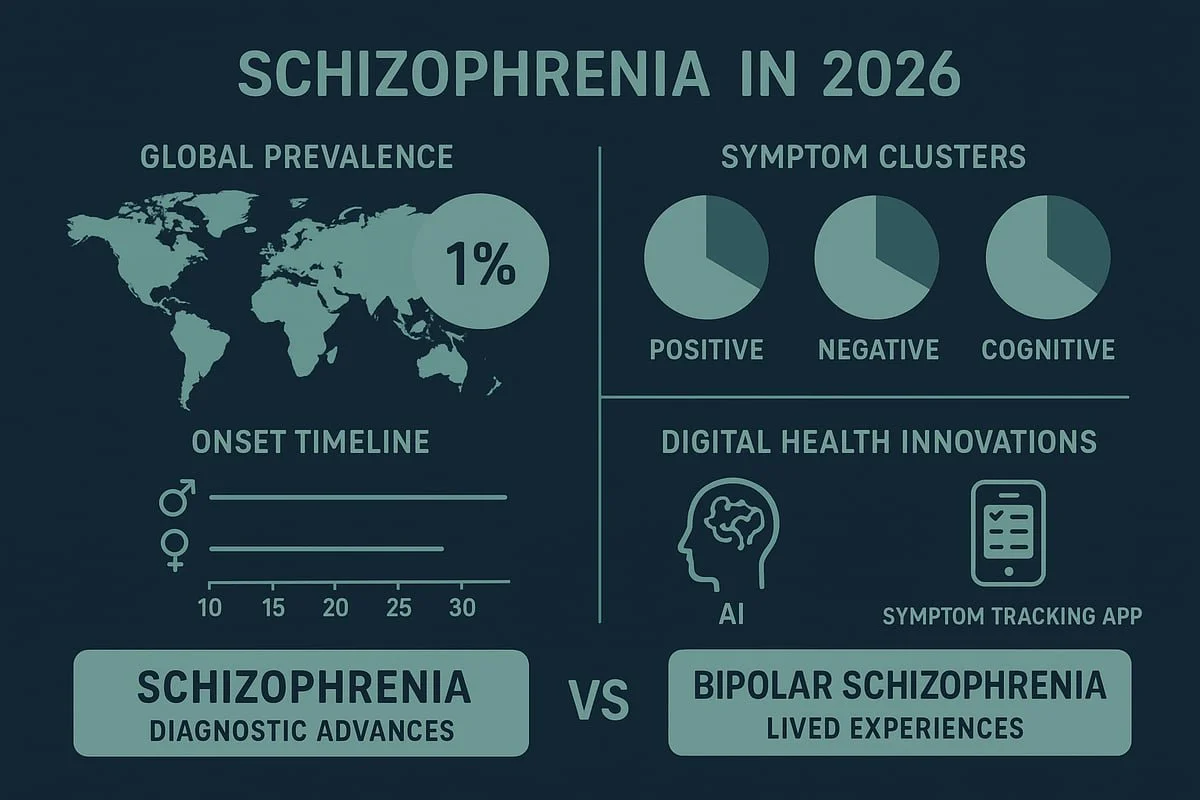
Schizophrenia is a severe, chronic psychotic disorder that disrupts thought, perception, and behavior. Affecting about 1% of the global population according to WHO estimates in 2025, it is marked by a profound break from reality, often referred to as psychosis.
Individuals with schizophrenia may experience hallucinations, delusions, or disorganized thinking. These symptoms can make daily functioning and social relationships challenging. Early intervention programs and digital tools, such as AI-driven symptom tracking, are becoming integral to care in 2026.
For example, a young adult might hear voices that others do not perceive and begin to withdraw from friends and family. The confusion between bipolar schizophrenia and primary psychotic disorders can make early diagnosis complex. Recent advances, including AI aids in diagnosing schizophrenia and bipolar disorder, are helping clinicians make more accurate distinctions between the two.
Types and Symptoms of Schizophrenia
Schizophrenia presents with a variety of symptoms, grouped into three main clusters:
Positive symptoms: Hallucinations (often auditory), delusions, and disorganized speech.
Negative symptoms: Reduced emotional expression, lack of motivation, and social withdrawal.
Cognitive symptoms: Impaired attention, memory, and executive function.
Historically, subtypes like paranoid or catatonic schizophrenia were recognized, but the DSM-5-TR no longer uses these categories. Instead, clinicians focus on the unique combination of symptoms present in each individual.
A common scenario is paranoid schizophrenia, where a person may believe others are out to harm them. Up to 80% of individuals experience auditory hallucinations. Negative symptoms, such as diminished motivation, often lead to greater disability than positive symptoms. The overlap with bipolar schizophrenia, especially when psychosis is present, continues to challenge practitioners.
Causes and Risk Factors
The development of schizophrenia is influenced by a complex interplay of genetics, neurobiology, and environment. Having a first-degree relative with schizophrenia confers a 10% risk, compared to the general population risk of 1%.
Neurodevelopmental factors play a significant role. Prenatal exposure to infections or complications during birth can increase vulnerability. Neurochemical imbalances, particularly involving dopamine and glutamate, are implicated in the disorder.
Environmental risk factors include urban upbringing and cannabis use during adolescence. Recent research highlights the role of epigenetic changes and immune system dysfunction. These factors are also being studied in relation to bipolar schizophrenia, as both conditions share some genetic and biological underpinnings.
Course, Prognosis, and Complications
Schizophrenia typically emerges in late adolescence or early adulthood, with men often developing symptoms in their late teens to early 20s and women in their late 20s to early 30s. The course is usually chronic, punctuated by episodes of acute psychosis.
Complications are significant. Individuals face high rates of unemployment, homelessness, and premature mortality, with life expectancy reduced by 10 to 20 years. Early intervention and coordinated specialty care are crucial, as they reduce relapse rates and improve quality of life.
Recovery is possible, especially when treatment begins promptly. For those with overlapping features of bipolar schizophrenia, longitudinal assessment is key to optimizing outcomes. Coordinated care models are making strides in supporting individuals on the path to recovery.
Bipolar Disorder vs. Schizophrenia: Key Differences
Understanding the key differences between bipolar schizophrenia presentations is essential for accurate diagnosis and effective care. Although these conditions can appear similar, their unique features profoundly impact treatment, prognosis, and day-to-day life.
Bipolar Disorder vs. Schizophrenia: Key Differences
Symptom Comparison
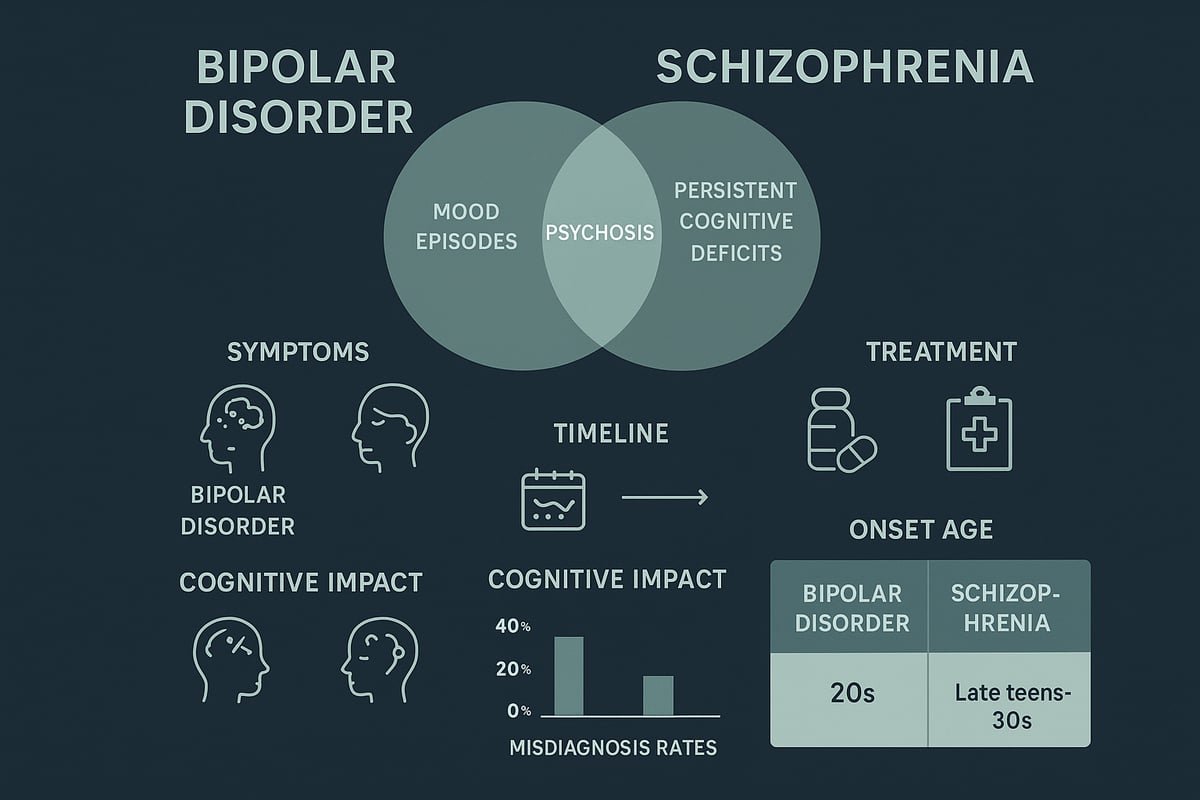
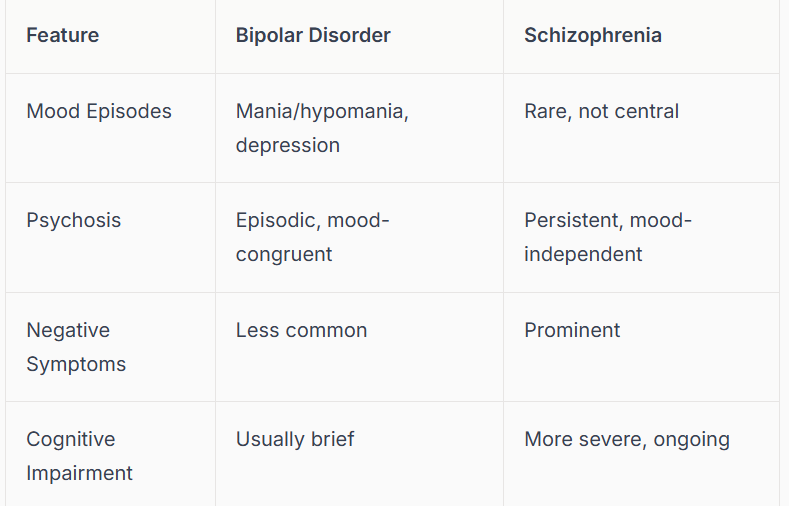
Both bipolar disorder and schizophrenia can present with psychosis, which leads to confusion in diagnosis. However, the symptom patterns, duration, and context differ. In bipolar schizophrenia cases, psychosis is usually tied to mood episodes, while in schizophrenia, it tends to be persistent and less influenced by mood.
Here is a comparison table of core symptoms:
comparison table of core symptoms
For example, a person with bipolar schizophrenia may experience hallucinations only during manic or depressive phases, while someone with schizophrenia may hear voices regardless of mood. The overlap of psychotic symptoms means up to 30% of cases are initially misdiagnosed. Recognizing these subtle variations is crucial for distinguishing between bipolar schizophrenia and other disorders.
Onset, Course, and Progression
The age of onset and illness trajectory differ between bipolar schizophrenia presentations and classic schizophrenia. Bipolar disorder often starts in late adolescence or early adulthood, with episodes lasting weeks to months. Individuals typically return to their baseline functioning between episodes.
In contrast, schizophrenia usually begins earlier in men and slightly later in women, with a more chronic and progressive course. Schizophrenia symptoms are often persistent, and functional recovery is less common. For example, someone with bipolar schizophrenia might return to work or studies after an episode, whereas a person with schizophrenia may struggle with ongoing symptoms.
Cognitive and Functional Impact
Cognitive deficits can occur in both bipolar disorder and schizophrenia, but the extent and persistence vary. In bipolar schizophrenia, cognitive problems are often temporary and linked to mood episodes. In schizophrenia, these deficits tend to be more enduring and substantially affect daily life.
Research comparing social cognition in schizophrenia vs. bipolar disorder shows that schizophrenia is associated with greater impairments, particularly in understanding others’ emotions and intentions. This impacts work, relationships, and independence. Bipolar schizophrenia may allow for periods of high functioning, while schizophrenia is more likely to result in long-term disability.
Diagnostic Challenges and Overlap
Distinguishing between bipolar disorder and schizophrenia is challenging due to overlapping features such as psychosis, mood instability, and impaired insight. The existence of schizoaffective disorder—a diagnosis with both mood and psychotic symptoms—adds further complexity.
Misdiagnosis is common, especially early in the course. Up to 50% of schizoaffective cases are initially classified as either bipolar schizophrenia or schizophrenia alone. Longitudinal assessment, structured interviews, and collateral information from family are essential tools for accuracy. Symptom rating scales and neuroimaging can support but not replace clinical judgment.
A key challenge is that symptoms may evolve over time, altering the diagnostic picture. Ongoing assessment and open dialogue remain vital for clarity.
Importance of Accurate Diagnosis
An accurate distinction between bipolar schizophrenia and schizophrenia is vital for guiding treatment and improving prognosis. Treatment regimens differ: bipolar disorder typically requires mood stabilizers, while schizophrenia relies on antipsychotics. Misdiagnosis can lead to inappropriate medication, unnecessary side effects, and poorer outcomes.
Early and precise diagnosis reduces stigma, supports tailored education, and helps families and professionals provide the right support. For example, labeling someone with schizophrenia instead of bipolar disorder may result in lifelong use of antipsychotics that are not always necessary. Multidisciplinary teams play a crucial role in ensuring comprehensive and accurate assessment for those affected by bipolar schizophrenia.
Diagnosis and Assessment in 2026
Accurate diagnosis is the cornerstone of effective care for bipolar schizophrenia and related conditions. In 2026, mental health professionals rely on a blend of updated criteria, technological innovations, and collaborative teamwork to ensure each individual receives the correct diagnosis and support.
Diagnosis and Assessment in 2026
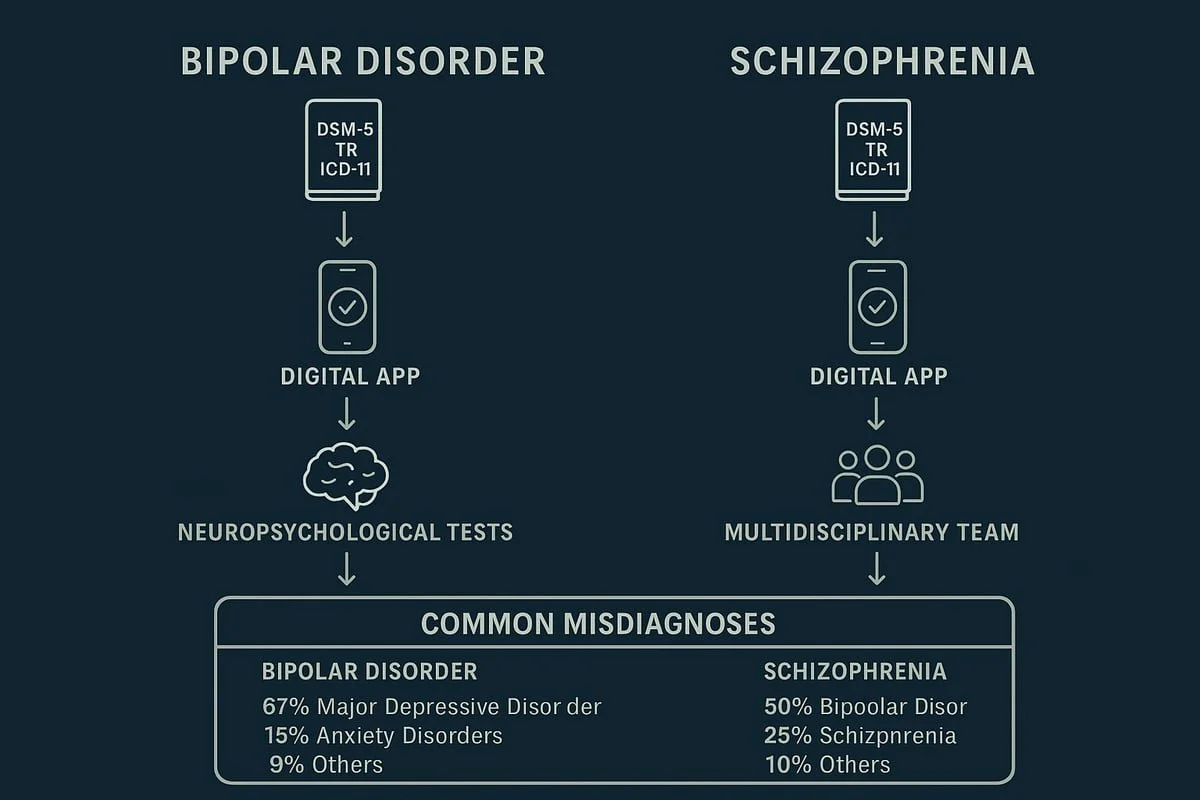
Modern Diagnostic Criteria and Tools
In 2026, clinicians use refined DSM-5-TR and ICD-11 standards to distinguish bipolar schizophrenia cases from other mental health disorders. Structured interviews, such as the SCID and MINI, provide a systematic approach to symptom assessment.
Digital health tools are now commonplace. Apps help patients track mood swings, psychotic episodes, and medication adherence. Neuropsychological testing offers quantitative insight into cognitive deficits, supporting the diagnostic process for bipolar schizophrenia.
Ongoing research into biomarkers, including neuroimaging and blood-based tests, holds promise but is not yet standard practice. These advancements help clinicians differentiate between overlapping symptoms, bringing greater clarity to complex cases.
Differential Diagnosis Process
Differentiating bipolar schizophrenia from other psychiatric and medical conditions requires a thorough, stepwise evaluation. Clinicians begin by ruling out medical causes, such as thyroid dysfunction or neurological disorders, which can mimic psychiatric symptoms.
A detailed family and developmental history is essential, as hereditary patterns often guide suspicion toward bipolar schizophrenia. Longitudinal observation allows professionals to track symptom evolution over time, capturing episodic or persistent patterns.
Collateral information from family or caregivers offers an external perspective, helping to clarify the context of mood or psychotic episodes. This comprehensive process minimizes misdiagnosis and directs individuals toward appropriate care.
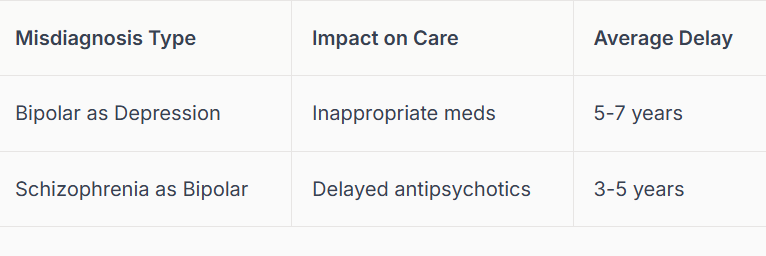
Common Misdiagnoses and Their Impact
Misdiagnosis remains a significant challenge in the assessment of bipolar schizophrenia. Symptoms such as severe depression, functional freeze, or psychosis can blur diagnostic boundaries. For instance, depressive states may be mistaken for primary mood disorders, while psychotic features could point to schizophrenia instead of bipolar disorder.
Consequences of misdiagnosis are profound: delayed treatment, inappropriate medication, and increased risk of morbidity. Exploring distinctions between depressive symptoms and other presentations, as described in Functional freeze vs. depression, highlights the need for careful evaluation.
Averages show that it can take 5-7 years to correctly identify bipolar schizophrenia, underlining the importance of ongoing reassessment and vigilance.
Common Misdiagnoses and Their Impact
Role of the Mental Health Team
Accurate diagnosis of bipolar schizophrenia relies on a multidisciplinary approach. Psychiatrists, psychologists, social workers, and primary care providers each contribute their expertise to the assessment and care plan.
Family involvement is encouraged, as loved ones often notice early warning signs or changes in behavior. Collaboration ensures that each aspect of the individual's experience is considered, leading to more precise diagnoses and better outcomes for those with bipolar schizophrenia.
Treatment Approaches: Bipolar Disorder vs. Schizophrenia
Understanding the treatment landscape for bipolar schizophrenia is crucial for improving outcomes. Both conditions require tailored, evidence-based interventions, but their management strategies differ in important ways. Let’s explore the latest approaches in 2026.
Bipolar Disorder Treatment Strategies
Managing bipolar schizophrenia involves a multi-pronged approach. Medications are the cornerstone, especially mood stabilizers like lithium and valproate. Atypical antipsychotics are often prescribed, particularly when psychotic features emerge. Antidepressants may be used cautiously to avoid triggering mania.
Psychotherapy is essential. Cognitive-behavioral therapy (CBT) helps individuals recognize mood changes and develop coping skills. Family-focused therapy and psychoeducation empower both patients and their loved ones.
Lifestyle interventions support stability. Regular sleep, stress management, and reduced substance use are vital for those with bipolar schizophrenia. Monitoring for medication side effects, such as thyroid or kidney issues with lithium, is standard practice.
Lithium’s unique benefit is its ability to reduce suicide risk by up to 60 percent, making it a frontline option for many living with bipolar schizophrenia.
Schizophrenia Treatment Strategies
Treatment for bipolar schizophrenia with predominant schizophrenia features centers on antipsychotic medications. Risperidone, olanzapine, and clozapine (for treatment-resistant cases) are commonly used in 2026. Side effect management, particularly metabolic and movement disorders, is a key concern.
Psychosocial interventions play a major role. Supported employment, skills training, and CBT for psychosis help improve functioning. Assertive community treatment (ACT) and coordinated specialty care provide wraparound support for those with bipolar schizophrenia.
Clozapine stands out for reducing suicide risk and improving outcomes in resistant cases. Monitoring for side effects, such as agranulocytosis, is essential. Addressing comorbid substance use and social isolation is also prioritized in schizophrenia-focused care.
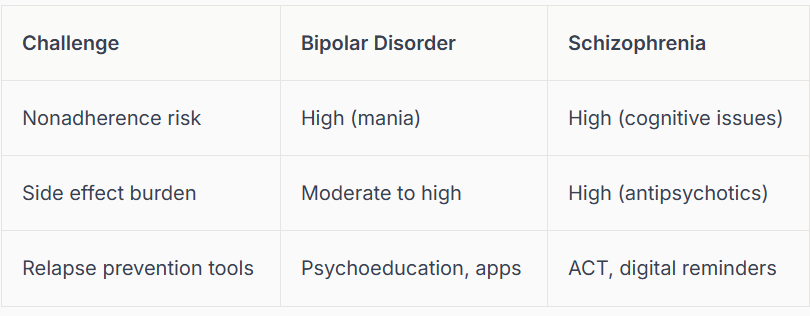
Comparing Treatment Challenges and Adherence
Bipolar schizophrenia presents distinct challenges when it comes to treatment adherence. For those with bipolar features, nonadherence often occurs during manic phases, when insight can be impaired. Side effects from mood stabilizers may further reduce compliance.
In schizophrenia, cognitive deficits and lack of insight are primary obstacles. Stigma and social withdrawal can make long-term engagement difficult. Relapse prevention requires a proactive approach, including early warning sign recognition and consistent medication.
Digital reminders and telehealth services have shown promise in improving adherence for both aspects of bipolar schizophrenia.
Innovations in Treatment (2026)
The landscape for treating bipolar schizophrenia continues to evolve. Digital therapeutics, such as mobile apps for mood and symptom tracking, are now integral to routine care. Virtual therapy platforms have expanded access, especially in underserved communities.
Pharmacogenomics allows clinicians to select medications based on genetic profiles, reducing trial and error. Long-acting injectable antipsychotics are increasingly used to support adherence in schizophrenia. Peer support and online communities foster engagement and resilience.
Emerging therapies are on the horizon. For instance, advances in schizophrenia treatments targeting muscarinic acetylcholine receptors promise more targeted symptom control. AI-driven relapse prediction tools have reduced hospitalizations by 20 percent, highlighting the role of technology in managing bipolar schizophrenia.
Family, Community, and Social Support
Support networks are essential for those managing bipolar schizophrenia. Psychoeducation for families reduces relapse rates and improves understanding. Community resources, such as housing and employment programs, play a vital role in recovery.
Peer-led groups offer acceptance and shared experience, reducing isolation. Public awareness campaigns are working to decrease stigma and promote inclusion. Holistic, recovery-oriented care—focusing on strengths, not just symptoms—remains the gold standard for bipolar schizophrenia support.
Family involvement is linked to a 50 percent lower relapse rate in schizophrenia, demonstrating the power of collaborative care in both conditions.
Living with Bipolar Disorder or Schizophrenia: Realities and Support
Lived Experience: Daily Challenges and Coping
Living with bipolar schizophrenia brings unique daily challenges. Many individuals struggle with unpredictable mood shifts, persistent symptoms, and the ongoing fear of relapse. Social isolation is common, with 60 percent of people with schizophrenia reporting it as a major barrier to well-being.
Work and relationships often become complicated, and stigma can lead to misunderstanding or discrimination. Socioeconomic factors, such as poverty, can make it even harder to access care or maintain stability. For more on this, see Mental health and poverty, which explores the impact of financial stress on recovery.
Peer support groups, structured routines, and self-monitoring are essential coping tools, helping individuals build resilience and hope.
Advice for Families and Caregivers
Families play a crucial role in supporting those with bipolar schizophrenia. Education is key: understanding symptoms, treatment options, and warning signs helps families respond effectively during crises. Open, nonjudgmental communication fosters trust and encourages individuals to seek help when needed.
Crisis planning, such as knowing what to do in emergencies or recognizing early warning signs, can prevent escalation. Joining caregiver support groups and accessing respite care provide much-needed relief and connection. Family psychoeducation has been shown to reduce caregiver burden and improve outcomes for both caregivers and individuals.
Empowerment and Recovery-Oriented Approaches
Empowerment is central to recovery for people living with bipolar schizophrenia. Focusing on strengths rather than limitations enables individuals to set meaningful goals and regain autonomy. Recovery is a personal journey, often supported by advocacy organizations and peer mentors who have walked similar paths.
Supported employment programs are especially impactful, doubling workforce participation rates for those with schizophrenia. These programs help individuals regain confidence, purpose, and community integration. Emphasizing empowerment helps shift the narrative from illness to possibility.
Reducing Stigma and Promoting Inclusion
Stigma remains a significant barrier for those with bipolar schizophrenia. Public education campaigns and open discussions about mental health are vital for dispelling myths and fostering inclusion. Legal protections and anti-discrimination laws also play a role in safeguarding rights.
Language matters: saying “person with schizophrenia” instead of labeling someone by their diagnosis promotes dignity and respect. National campaigns in 2025 led to a 15 percent decrease in reported stigma, showing progress is possible. Understanding mood fluctuations, such as those described in Fall mental health and SAD, can further public awareness and empathy.
Future Directions and Research in Bipolar Disorder and Schizophrenia
The future of bipolar schizophrenia research is rapidly evolving, with breakthroughs reshaping our understanding and treatment of these complex conditions. Research teams worldwide are uncovering new biological markers, refining diagnostic tools, and developing targeted therapies. These advances promise more accurate diagnoses, effective interventions, and improved quality of life for those affected by bipolar schizophrenia and related disorders.
Advances in Understanding and Treatment
Genetic studies have identified risk genes linked to bipolar schizophrenia, enabling the creation of polygenic risk scores for earlier identification. Neuroimaging is mapping brain circuits involved in mood and psychotic symptoms, helping to distinguish between overlapping features. Researchers are also making strides in finding biological markers that could lead to objective diagnostic tests, such as blood-based inflammatory markers.
Understanding the relationship between hormonal imbalances, inflammation, and mood disorders is crucial. For example, studies on conditions like PCOS provide insight into how hormonal factors intersect with mood symptoms, highlighting the complexity of bipolar schizophrenia. For more on this intersection, see the PCOS and depression link.
Personalized and Precision Medicine
Personalized medicine is reshaping how clinicians approach bipolar schizophrenia. Treatment is increasingly tailored to each individual’s genetic, biological, and lifestyle profile. Pharmacogenomics helps match medications to a person’s metabolism, reducing side effects and improving outcomes.
Predictive analytics and digital phenotyping are now used to forecast mood episodes or psychotic relapses. For example, smartphone data can detect early warning signs of mania or psychosis days before symptoms become severe. These early interventions are crucial for preventing hospitalizations and supporting long-term recovery in bipolar schizophrenia.
Emerging Therapies and Technologies
Innovations in bipolar schizophrenia treatment include new medications targeting glutamate pathways and inflammation. Digital therapeutics, such as mobile apps and online platforms, offer symptom monitoring and virtual therapy, making mental health support more accessible.
Brain stimulation techniques like transcranial magnetic stimulation (TMS) are being studied for both bipolar and schizophrenia symptoms. Virtual reality-based social skills training is helping individuals practice interactions in a safe, controlled environment. These tools are expanding the options available for managing bipolar schizophrenia.
Societal and Policy Implications
As science advances, policy must keep pace to ensure equitable access to care for people with bipolar schizophrenia. Expanding insurance coverage for innovative treatments, including digital and pharmacogenomic approaches, is essential. Integrating mental health services into primary care and community programs supports early detection and intervention.
Advocacy organizations continue to push for research funding and public education. For example, coordinated specialty care programs are expanding in 2026, providing comprehensive support for those living with bipolar schizophrenia. These efforts help close treatment gaps and promote long-term recovery.
Local Support |
PA, NC & SC
Mariah J. Zur | Therapy Intensives in Raleigh, Pittsburgh and across NC, SC, PA
I offer focused therapy intensives for adults who are still functioning but feel worn down by constant pressure, anxiety, or patterns that no longer work. This work is designed for people who want depth, clarity, and relief without labels or long-term weekly therapy. If you’re in North Carolina, South Carolina, or Pennsylvania and curious whether an intensive format could be supportive, you’re welcome to learn more.
Join me on Facebook, Instagram, Pinterest, Google orTikTok for more educational tips, trauma recovery insights, and updates on therapy intensives in Pennsylvania, North Carolina, and South Carolina.
Disclaimer
The content shared here is for educational and informational purposes only. It is not a substitute for psychotherapy, medical care, or individualized mental health treatment. Reading this blog or engaging with my content does not establish a therapeutic relationship.
If you are experiencing significant distress or feel you need personalized support, I encourage you to seek care from a licensed mental health professional in your state. Therapy is deeply personal, and the right support should be tailored to your specific needs, pace, and circumstances.
For adults located in North Carolina, South Carolina, or Pennsylvania who are seeking focused, confidential support, I offer customized therapy intensives designed to address chronic stress, internal pressure, and patterns that no longer work. Information about these services can be found throughout this site.
About the Author
Mariah Zur, LPC is a licensed therapist who works with high-achieving adults navigating chronic stress, internal pressure, and the quiet unraveling that can happen beneath outward success. Her work is especially suited for individuals who are highly functional, deeply self-aware, and exhausted from holding everything together.
Mariah offers therapy intensives for adults seeking focused, contained support without labels, long-term weekly therapy, or unnecessary exposure. Her approach is grounded, relational, and nervous-system informed, helping clients slow the internal spiral, regain a sense of control, and move forward with clarity and steadiness.
She provides intensive therapy services online across North Carolina, South Carolina, and Pennsylvania, with in-person options available in Raleigh, NC.
Credentials
Mariah J. Zur, MS, LPC
Licensed Professional Counselor
Doctoral Student, Counselor Education and Supervision