Professional Trauma Guide: Expert Strategies for 2026
The demand for professional trauma expertise is reaching new heights in 2026 as trauma care becomes more urgent and complex than ever before. With evolving trauma types and rising expectations for rapid, evidence-based support, trauma professionals face mounting pressure to deliver the best possible outcomes.
This guide offers expert strategies designed to help you elevate your professional trauma practice in today’s dynamic landscape. You will discover how to understand trauma in 2026, apply cutting-edge interventions, access essential tools and certifications, and implement practical steps that drive real impact.
New research and digital tools are transforming trauma response. Are you ready to become a leader in trauma care? Explore actionable strategies here and take your professional trauma expertise to the next level.
The Evolving Landscape of Trauma in 2026
The landscape of professional trauma is shifting rapidly as we move into 2026. Today’s trauma professionals face an environment shaped by complex challenges, new research, and the increasing need for specialized expertise. The very definition of trauma now encompasses more than individual incidents, requiring a comprehensive approach to care and intervention.
Defining Trauma: Beyond the Basics
In 2026, professional trauma experts recognize trauma as a multidimensional experience. The definition now extends beyond acute events to include complex trauma, developmental trauma, and collective trauma experienced by entire communities.
Recent CDC data from 2025 shows a substantial rise in trauma-related diagnoses following the pandemic. This increase highlights the urgent need for professional trauma expertise. Trauma professionals must now assess the effects of not only personal adversity but also ongoing social, environmental, and digital stressors.
For example, climate-related disasters are causing widespread mental health impacts. Communities affected by wildfires, floods, and hurricanes report rising cases of trauma symptoms, especially among children and older adults.
The intersection of trauma with chronic stress, anxiety, and professional burnout is increasingly apparent. New diagnostic criteria and updates in the DSM are reshaping how professional trauma is identified and treated, ensuring care is evidence-based and responsive to evolving needs.
Insights from military and emergency response sectors are influencing civilian trauma protocols. Tools and strategies once confined to crisis zones are now being adopted in hospitals, schools, and workplaces. For an in-depth look at current data and best practices, the 2024 ESO Trauma Index Report offers valuable benchmarks for trauma professionals seeking to enhance their approach.
The scope of professional trauma care now includes a broader array of experiences, demanding that every practitioner stays current with diagnostic and intervention advances.
Emerging Trends and Challenges
The professional trauma field in 2026 is marked by growing diversity. Trauma professionals are working with clients from a wide range of cultural, generational, and identity backgrounds. Each population brings unique perspectives and needs, requiring culturally competent care.
Technology and social media are now double-edged swords in trauma recovery. While they provide rapid access to support and resources, they also increase exposure to distressing events. Telehealth and remote interventions have become essential tools for professional trauma specialists, particularly when reaching rural or underserved communities.
One critical challenge is the rising prevalence of vicarious trauma among professionals themselves. According to the NIH, 40% of healthcare workers reported secondary traumatic stress in 2025. As trauma events become more frequent and complex, protecting the well-being of trauma professionals is vital.
Barriers to access remain significant. Marginalized communities, rural populations, and those affected by systemic inequities often face delays in receiving professional trauma care. Real-world examples, such as responses to recent hurricanes and wildfires, demonstrate both the strengths and limitations of current systems.
To navigate these emerging trends, trauma professionals must remain adaptable, informed, and committed to ongoing development. The evolving landscape demands a proactive approach to both individual and collective trauma, ensuring that care is accessible, effective, and grounded in the latest research.
Expert Strategies for Trauma Assessment and Intervention
Effectively assessing and intervening in trauma is at the heart of every professional trauma practice. As trauma presentations grow more complex, professionals must master advanced techniques and evidence-based strategies. This section explores the latest approaches, from comprehensive assessments to cutting-edge interventions, and provides a practical, stepwise guide for implementation.
Advanced Trauma Assessment Techniques
Today’s professional trauma assessment goes far beyond surface symptoms. Clinicians utilize comprehensive screening tools, such as the Trauma Symptom Checklist and structured interviews, to capture the full scope of a client's experience. These tools help professionals identify overlooked trauma types, including developmental and collective trauma.
Neurobiological markers and physiological assessments are increasingly integrated into trauma evaluations. Biometrics like cortisol levels, heart rate variability, and sleep patterns offer measurable insights into trauma’s impact on the body. This data-driven approach allows professional trauma practitioners to tailor care with greater precision.
Cultural competence now plays a central role in trauma assessment. Professionals must recognize how cultural backgrounds, language, and community norms shape trauma responses. The ACEs (Adverse Childhood Experiences) framework, for example, has been successfully adapted for diverse populations, ensuring assessments are inclusive and meaningful.
Digital tools have transformed assessment accessibility. Telehealth platforms and secure apps enable remote screening, making it easier for professional trauma specialists to reach clients in underserved areas. According to the APA in 2025, early assessment using these advanced methods is linked to 30 percent better long-term outcomes.
All these strategies empower professional trauma providers to identify challenges early and set the stage for effective intervention.
Evidence-Based Interventions for 2026
Professional trauma intervention in 2026 is rooted in robust research and innovation. Top modalities remain central, with Eye Movement Desensitization and Reprocessing (EMDR), Internal Family Systems (IFS), Somatic Experiencing, and Trauma-Focused Cognitive Behavioral Therapy (CBT) leading the way. Each offers unique pathways to healing, whether addressing intrusive memories or restoring a sense of safety.
Innovations in brief and intensive therapy formats are transforming care delivery. Many professionals are now exploring whether therapy intensives or weekly sessions best meet client needs, optimizing results while respecting time constraints. Group and community-based interventions are also gaining ground, offering peer support and collective healing for trauma survivors.
Body-based therapies, such as mindfulness and somatic practices, have become essential. In fact, 65 percent of professional trauma practitioners now incorporate somatic methods, reflecting mounting evidence for their effectiveness. If you are interested in deepening your body-based practice, consider exploring somatic tools for generational trauma, which offers valuable insights and practical techniques.
Special populations require tailored strategies. Children, first responders, and survivors of systemic trauma benefit from interventions adapted to their unique needs. Military-grade trauma kits and protocols, once exclusive to emergency settings, are now being adopted in civilian trauma care, further expanding the professional trauma toolkit.
These interventions, when matched to client needs, can significantly improve outcomes and support long-term recovery.
Step-by-Step Guide: Implementing Trauma Interventions
To ensure successful outcomes, every professional trauma provider should follow a structured, stepwise approach to intervention:
Initial Assessment and Risk Evaluation
Begin with a thorough assessment, using both standardized tools and clinical judgment. Identify immediate risks and the full spectrum of trauma experiences.Collaborative Treatment Planning
Engage clients in setting goals and preferences. Professional trauma care thrives on shared decision-making, which increases engagement and trust.Selecting and Tailoring Interventions
Choose interventions that best fit the client’s needs, culture, and trauma history. Adapt modalities as new information emerges throughout the process.Ongoing Monitoring and Adjustment
Regularly review progress with clients, adjusting strategies as needed. Digital tools can help track outcomes and flag concerns early.Building Resilience and Post-Traumatic Growth
Support clients in developing resilience skills and recognizing growth. Professional trauma work is as much about fostering strengths as it is about healing wounds.
By following these steps, professional trauma practitioners can deliver care that is ethical, personalized, and effective. The field continues to evolve, but these foundational practices remain essential for measurable, lasting impact.
Tools, Resources, and Certifications for Trauma Professionals
Staying at the forefront of professional trauma care in 2026 requires access to the right tools, resources, and certifications. As trauma presentations become more complex, having a comprehensive toolkit and ongoing training is essential for effective, rapid-response care.
Essential Trauma-Informed Tools and Kits
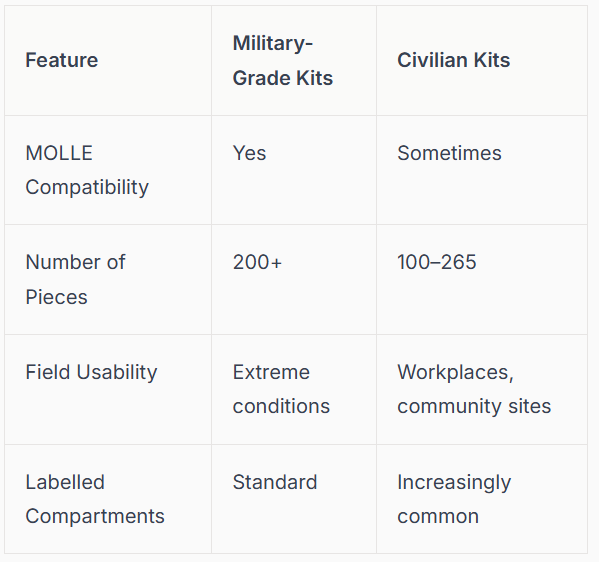
For professional trauma response, a robust first aid kit is indispensable. In 2026, both military-grade and civilian trauma kits are designed for speed, organization, and adaptability. The best kits feature labeled compartments, MOLLE systems for easy attachment, and supplies for a range of injuries.
A comparison of key features:
For example, a 265-piece trauma kit is now standard in many workplaces, supporting rapid intervention during emergencies. Digital resources also play a vital role in professional trauma care. Apps for trauma assessment, telehealth platforms, and online communities provide real-time support and knowledge sharing.
Workplaces have seen a 50% increase in trauma kit adoption, reflecting the rising need for preparedness. For any professional trauma setting, selecting the right tools can make a measurable difference in outcomes.
Professional Development: Certifications and Training
Certifications are central to professional trauma expertise. Leading credentials include Certified Trauma Professional (CTP), Clinical Trauma Professional, Internal Family Systems (IFS), and EMDR certifications. Each offers unique benefits, from deepening clinical skills to enhancing credibility with clients and employers.
Requirements for 2026 often include a blend of coursework, supervised clinical hours, and regular renewal. Ongoing education is vital, as new research and intervention methods continue to emerge. Programs like Evergreen Certifications have raised standards industry-wide, with 70% of trauma professionals now pursuing advanced certifications.
When choosing a certification pathway, align your choice with your career goals and the populations you serve. For those seeking specialized training, Trauma-informed courses for professionals offer a comprehensive overview of options and requirements.
Investing in professional trauma certifications not only sharpens your clinical edge but also demonstrates commitment to best practices, ensuring the highest level of care for clients.
Building a Trauma-Informed Practice: Key Considerations
Integrating trauma-informed principles into every aspect of professional trauma practice is no longer optional—it is essential. This approach starts with understanding how trauma impacts individuals, families, and organizations. It extends to creating policies that prioritize safety, inclusivity, and empowerment.
Organizational support is a cornerstone. Team-wide training ensures that everyone, from clinicians to administrative staff, understands trauma-informed care. Safe, inclusive environments foster trust and promote healing for both clients and professionals.
Real-world examples include trauma-informed policies in schools, hospitals, and workplaces. These organizations report a 45% higher client satisfaction rate, underscoring the tangible benefits of a trauma-informed approach.
Building a sustainable, professional trauma practice means ongoing reflection, policy updates, and a commitment to staff well-being. This foundation allows professionals to deliver the best possible care and adapt as trauma care evolves.
Innovations and Future Directions in Trauma Care
The landscape of professional trauma is advancing rapidly as technology and holistic practices reshape both assessment and intervention. To remain at the forefront, professionals must embrace these innovations while preparing for emerging challenges and opportunities.
Technology and Digital Innovations
Cutting-edge technology is revolutionizing professional trauma assessment and treatment. Artificial intelligence is now capable of analyzing patient histories, predicting risk factors, and even supporting therapeutic conversations. For instance, the Thousand Voices of Trauma Dataset is enabling researchers to train AI systems for prolonged exposure therapy, offering scalable solutions for trauma professionals.
Virtual reality and augmented reality have emerged as powerful tools for immersive therapy. VR exposure therapy, especially for PTSD among veterans and first responders, has led to a 30% increase in positive outcomes with tech-assisted interventions according to recent NIH data. Mobile health apps now deliver real-time support, symptom tracking, and crisis intervention, making professional trauma care more accessible than ever.
Here is a comparison of key digital tools:
InnovationApplicationReported ImpactAI & Machine LearningRisk assessment, therapy supportFaster, more precise careVR/ARExposure therapy simulationsImproved PTSD outcomesmHealth AppsProgress tracking, telehealthGreater access, engagement
As technology continues to evolve, professional trauma specialists must remain adaptive, integrating these tools to enhance client outcomes.
Integrative and Holistic Approaches
In 2026, professional trauma care recognizes the need for mind, body, and environmental healing. Traditional therapies are now complemented by integrative modalities, providing a holistic framework for recovery.
Popular approaches include:
Trauma-informed yoga and movement therapies
Mindfulness-based stress reduction
Nutritional support for mental health
Expressive arts and creative therapies
Somatic therapies, rooted in neuroscience, are increasingly evidence-based and effective in restoring regulation after trauma. Programs emphasizing polyvagal theory help clients reconnect with their bodies and foster resilience.
Community settings are adopting trauma-informed yoga and mindfulness groups, making professional trauma support more accessible to diverse populations. The integration of these modalities not only addresses symptoms but also empowers clients to achieve post-traumatic growth. As research advances, professionals are encouraged to blend these holistic practices with established interventions for optimal results.
The Future of Trauma Professionalism
The future of professional trauma is defined by collaboration, innovation, and advocacy. Interdisciplinary care models are becoming standard, uniting clinicians, nurses, social workers, and peer specialists for comprehensive support.
Legislative advancements and trauma-informed policies are reshaping schools, workplaces, and healthcare systems. Professionals must prepare for new trauma types, including climate-related and digital trauma, by pursuing ongoing education and specialized training.
Effective professional trauma practice also demands a commitment to self-care and organizational well-being. Without adequate support, 60% of trauma professionals report burnout risk. Team-based excellence, as highlighted by the Trauma Quality Improvement Program's 15-Year Milestone, demonstrates the power of shared learning and innovation.
Looking ahead, trauma professionals who embrace change, foster resilience, and advocate for systemic transformation will lead the field with confidence.
Step-by-Step Roadmap: Becoming a Trauma Expert in 2026
Becoming a leader in professional trauma care requires a structured, intentional approach. This roadmap outlines the core steps to elevate your skills, credibility, and impact in trauma care for 2026. Each step is designed to build your expertise, ensuring you meet the demands of a dynamic, evolving field.
Step 1: Foundational Education and Self-Assessment
The first step to becoming a professional trauma specialist is clarifying your motivation and strengths. Self-assessment tools, such as reflective questionnaires or skills inventories, help you evaluate readiness for specialized trauma work.
Pursue foundational education through accredited degrees in psychology, social work, or nursing. Specialized trauma coursework and introductory certifications strengthen your base. If you are transitioning from general mental health, map your transferable skills and identify knowledge gaps.
Use self-assessment checklists to gauge fit.
Research trauma-focused graduate programs.
Seek mentors who practice professional trauma care.
Early investment in your education lays the groundwork for advanced growth.
Step 2: Gaining Practical Experience
Hands-on experience is essential for professional trauma competence. Begin with supervised clinical hours in settings that expose you to diverse trauma populations. Join trauma response teams or volunteer during disaster relief to expand your perspective.
Mentorship accelerates learning, offering real-time feedback and support. Engage in community initiatives like school-based interventions or crisis hotlines. These practical opportunities deepen your understanding of trauma's impact and the nuances of care.
Log clinical hours in trauma-focused environments.
Volunteer with local or national relief organizations.
Participate in peer consultation groups.
Building a varied clinical portfolio is vital for a robust professional trauma foundation.
Step 3: Pursuing Advanced Certifications
Advanced certifications signal your commitment to excellence in professional trauma care. Programs like Certified Trauma Professional, EMDR, or the Trauma Nursing Core Course provide specialized skills and credibility.
Understand application requirements, costs, and renewal timelines for each credential. Select certifications aligned with your career goals, such as clinical trauma work, emergency response, or leadership roles. For nurses, the Trauma Nursing Core Course Details offer evidence-based protocols and systematic assessment training.
Compare certification pathways in a table to clarify options.
Track renewal deadlines to maintain active status.
Pursue continuing education for evolving best practices.
Ongoing certification elevates your professional trauma profile and expands your impact.
Step 4: Mastering Intervention Techniques
Deepen your expertise in evidence-based modalities central to professional trauma care. Focus on approaches like EMDR, Somatic Experiencing, and Internal Family Systems. For a comprehensive overview, see this Internal Family Systems introduction.
Attend advanced workshops, join peer consultation groups, and integrate digital tools into your practice. Evaluate your outcomes regularly and adapt interventions to meet each client's needs.
Participate in specialized training for new techniques.
Use outcome measures to refine your approach.
Stay informed on emerging research.
Mastering intervention skills is key to delivering measurable results in professional trauma settings.
Step 5: Building and Sustaining a Trauma-Informed Practice
Sustaining excellence in professional trauma requires more than clinical skill. Develop ethical, client-centered care standards and trauma-informed policies for your organization. Prioritize self-care, supervision, and ongoing professional development to avoid burnout.
Implement trauma-informed supervision and team wellness programs. Plan for long-term career growth by setting leadership goals and staying engaged with professional communities.
Create safe, inclusive environments for clients and staff.
Advocate for trauma-informed policies in your workplace.
Regularly review and update practice standards.
By following this roadmap, you position yourself as a leader in professional trauma care, ready to meet the challenges and opportunities of 2026.
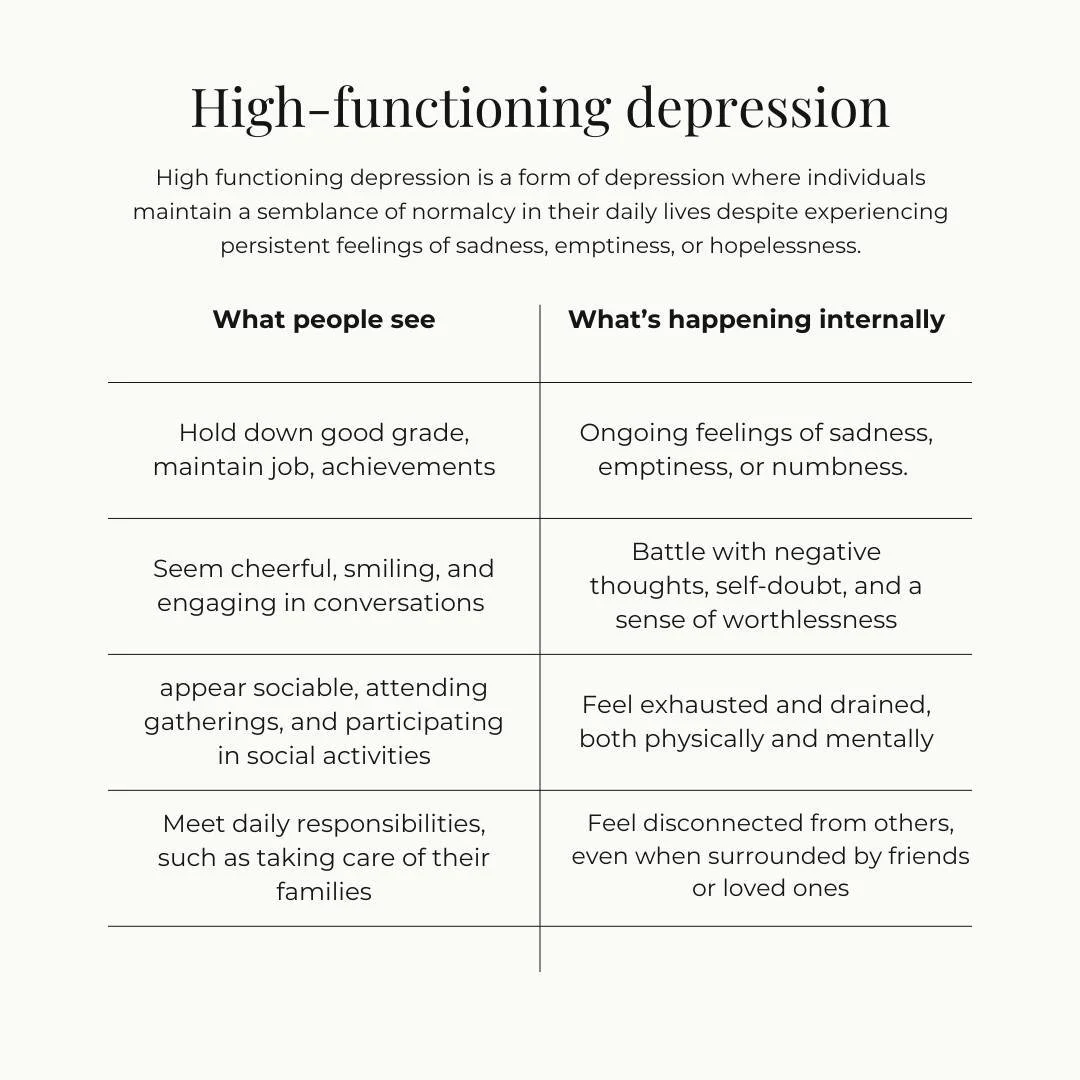
Mariah J. Zur, LPC is a licensed therapist based in Raleigh, North Carolina, specializing in intensive therapy for high-achieving adults experiencing chronic stress, internal pressure, and high functioning anxiety. She works primarily with executives, entrepreneurs, physicians, attorneys, and founders who remain outwardly successful but feel worn down by constant overdrive.
Mariah’s work is especially suited for professionals navigating burnout, decision fatigue, and emotional disconnection despite insight and coping skills. She offers focused therapy intensives designed to create meaningful change without long-term weekly therapy or diagnostic labeling.
She provides intensive therapy services for adults across North Carolina, with in-person options available in Raleigh and the Research Triangle, and works with clients statewide through structured intensive formats.
Credentials:
Mariah J. Zur, MS, LPC
Licensed Professional Counselor
Doctoral Student, Counselor Education and Supervision