Functional Freeze vs. Burnout vs. Depression: Why You Feel Stuck (But Still Functioning)
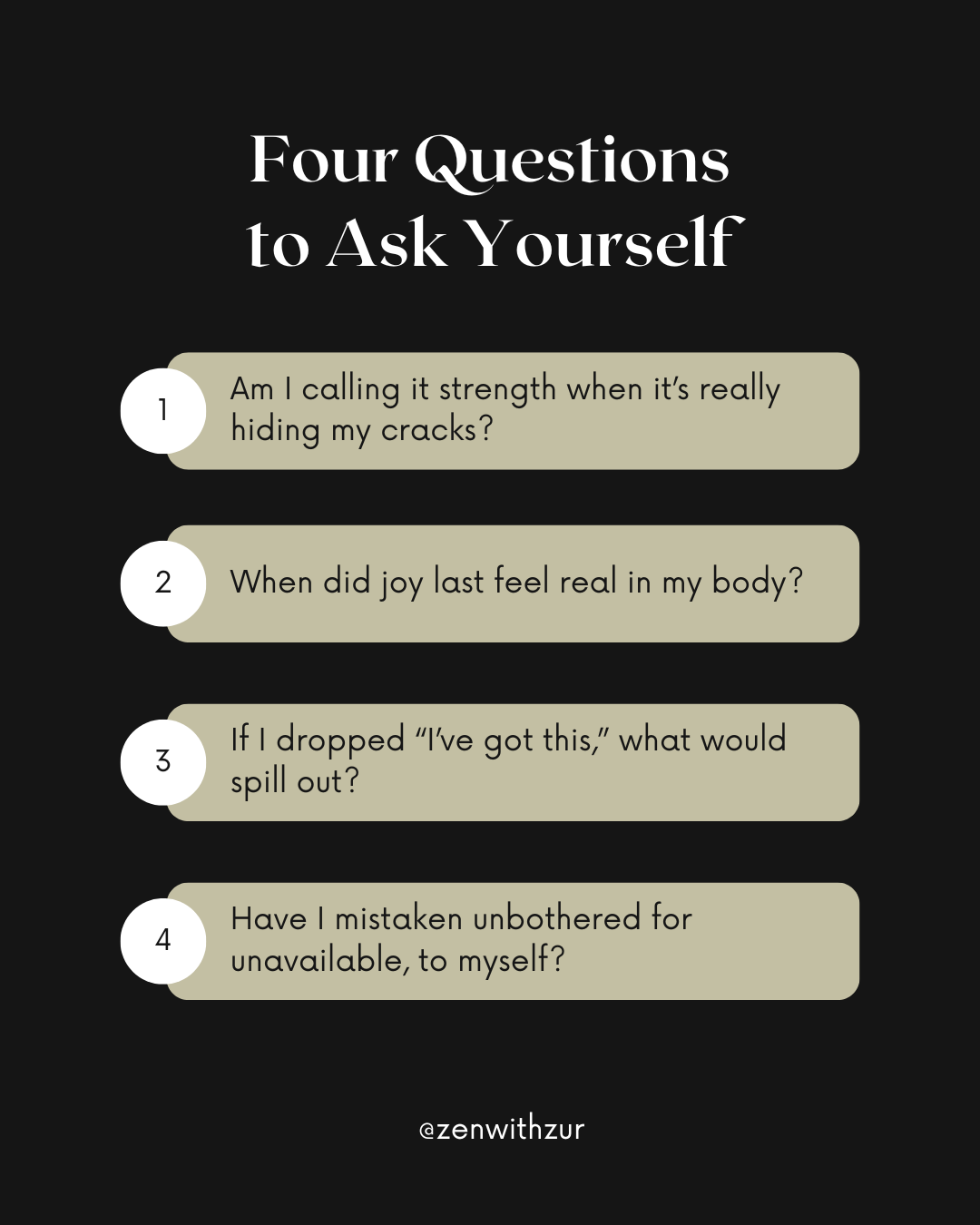
When “strong” starts feeling like numb, it’s not strength, it’s survival mode. High-achieving women know this mask too well: holding it together, pushing through, smiling while your body forgets joy. This isn’t weakness, it’s burnout. Time to rewrite what strength really means.
When “Strong” Feels Like Numb
You’re hitting deadlines, managing kids, answering texts. From the outside, you look like you’ve got it together. Inside, it’s a different story:
You feel flat, like life is muted.
Joy feels far away.
Rest doesn’t actually recharge you.
People call you “so strong.” But you know the truth: I don’t feel strong. I feel dead inside.
That’s not weakness. It’s not laziness. It’s not “just stress.” More often, it’s what I call functional freeze—a nervous system stuck in survival mode.
Let’s break down how functional freeze differs from burnout and depression, so you can stop gaslighting yourself and start healing.
What Is Functional Freeze?
Functional freeze is a trauma response, a nervous system survival state described in polyvagal theory as the dorsal vagal shutdown.
Think of it as a half-alive mode: your body is still moving, but your energy, presence, and joy have gone offline.
Signs of functional freeze:
Numbness or disconnection (“I can’t feel much of anything”).
Constant overthinking without action.
Exhaustion no amount of sleep fixes.
Going through the motions but not feeling alive.
Functional freeze is common in high-achieving women who grew up in homes where stillness, emotion, or rest weren’t safe.
Burnout vs. Functional Freeze
Burnout comes from chronic workplace or caregiving stress. It’s exhaustion after running too long on empty.
Freeze is different: it’s your nervous system slamming the brakes, saying “No more—we shut down now.”
Burnout feels like: drained energy, irritability, dread about tasks.
Freeze feels like: numb, blank, foggy—like someone unplugged you.
Burnout recovers with rest. Freeze often doesn’t.
Depression vs. Functional Freeze
Depression and freeze overlap—but they’re not identical.
Major Depression (MDD):
Persistent low mood for at least 2 weeks.
Loss of interest/pleasure.
Sleep, appetite, energy shifts.
Can affect every area of life.
Freeze:
May not include sadness—just numbness.
Can switch states quickly if safety is restored.
Feels more like “absent” than “hopeless.”
Key difference: Depression is a clinical disorder. Functional freeze is a state of the nervous system. You can have both, but knowing the difference changes how you heal.
Why Naming the Right State Matters
When you don’t know what’s happening, you call yourself lazy, broken, or unmotivated.
But freeze isn’t failure—it’s protection. It’s your body saying: “I don’t feel safe enough to show up fully.”
Naming the state lets you shift from self-blame → self-compassion.
Quick Tools to Shift From Freeze
Small steps, not huge leaps, are what tell your body it’s safe again:
Orienting: Slowly look around and name 5 colors. Your body remembers you’re here, not back there.
Wall push: Push against a wall for 60 seconds. It reactivates muscles, reminding your body you can move.
Humming or “vooo”: Vibrations stimulate the vagus nerve, easing shutdown.
Micro-rest: 2–5 minutes of non-productive stillness (yes, you’ll feel twitchy at first).
Personal Perspective
I know this state well. In my 30s, I looked like I had everything together—but I was running on empty inside. Rest felt unsafe. Boundaries felt selfish. Joy felt like a trap.
It wasn’t until I learned to spot freeze for what it was that healing began. Somatic tools gave me an entry point back into my body. IFS helped me meet the parts that were terrified of slowing down. Naming it changed everything.
Why It Matters for Generational Trauma
Freeze often isn’t just “your problem”—it’s an inherited pattern. If your family survived by working harder, staying silent, or shutting down emotions, your nervous system likely learned to do the same.
The cycle can stop with you. But it doesn’t stop by pushing harder. It stops by learning to feel safe enough to soften.
FAQs About Functional Freeze, Burnout, and Depression
What is functional freeze?
Functional freeze is a trauma response where your nervous system shuts down to survive. You can still function outwardly, but inside you feel numb, foggy, or detached.
How is burnout different from freeze?
Burnout comes from chronic stress and often improves with rest. Freeze is the body’s emergency shutdown and doesn’t resolve with simple rest—it needs nervous system support and safety cues.
How is functional freeze different from depression?
Depression is a diagnosable mental health condition with persistent sadness and loss of pleasure. Functional freeze is a nervous system state of numbness and shutdown. You can have both, but treatment approaches differ.
What causes functional freeze?
Freeze often develops from childhood trauma, neglect, or chronic stress. It can also be inherited as a survival pattern from previous generations.
How do you get out of functional freeze?
Small somatic practices help: orienting, wall pushes, humming, or micro-movements. Working with a trauma-informed therapist (IFS, somatic therapy) provides deeper, lasting healing.
If you’ve made it this far…
Functional freeze is common and reversible. Whether it’s worsened by trauma, ADHD, or seasonal shifts, you can thaw your nervous system with small, repeated, bottom-up actions supported by IFS and somatic therapy.
If your brain keeps calling you lazy, but your body feels like it’s moving through wet cement, that’s not a character flaw. It’s a nervous system doing its best to protect you.
I help high-functioning women in their 30s understand and work with their functional freeze symptoms using IFS, somatic tools, and nervous system mapping.
You don’t have to “push harder.” You just need a different way through. Schedule with me now to learn How to Get Out of Freeze Trauma Response.
Trauma therapist in Pittsburgh, Philadelphia, Erie, Harrisburg and across Pennsylvania. Accepting new clients for trauma intensives.
If you’re struggling to move forward from a toxic relationship, let’s work together. I offer online trauma therapy and intensives across Pittsburgh, Harrisburg, Erie, Philadelphia, and all of Pennsylvania.
Join me on Facebook, Instagram, Pinterest, Google orTikTok for more educational tips & updates!
Disclaimer: Listen, what you see here on my blog or social media isn’t therapy, it’s meant to educate, inspire, and maybe even help you feel a little less alone. But if you’re in it right now and need real support, please reach out to a licensed therapist in your state who can walk alongside you in your healing journey. Therapy is personal, and you deserve a space that’s all about you. If you’re in PA and looking for a trauma therapist who gets it, I’m currently accepting new clients for trauma intensives. Let’s fast-track your healing journey, because you deserve to feel better, sooner.
About the Author: Mariah J. Zur, LPC is a trauma-informed therapist based in Pennsylvania, specializing in childhood trauma recovery, emotional healing, and helping individuals break free from toxic relationship patterns. With over 10 years of experience, Mariah uses evidence-based approaches like Internal Family Systems (IFS) therapy and trauma intensives to guide her clients through their healing journey. Passionate about empowering women to reclaim their emotional freedom, Mariah provides virtual and in-person therapy in Pittsburgh, Philadelphia and across Pennsylvania. When she's not in the therapy room, she’s advocating for mental health awareness and supporting others in their personal transformation.
Research Brief Author: Mariah J. Zur, M.S., LPC, CCTP.
If you’re living in functional freeze, you’re not broken. You’re carrying a nervous system strategy that once kept you safe. Naming it is the first act of compassion. Shifting it is the first act of freedom.